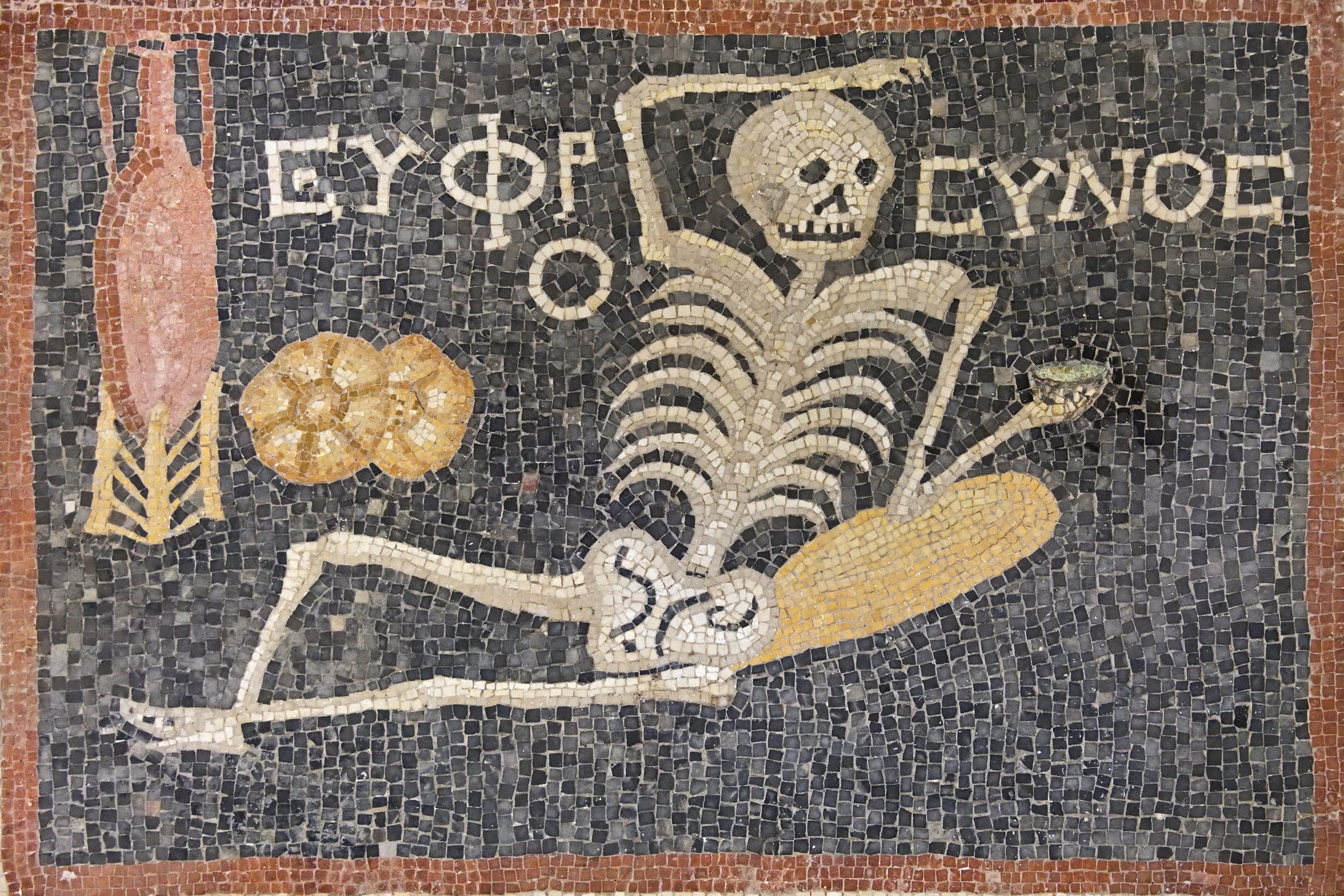
Everyone dies sometime. But when and how? Those questions become more salient as birthdays roll by. It has been said that wherever old people gather there is an ‘organ recital’ of malfunctioning body organs and parts. I, too, have a recital.
Last year, at age 88, I woke up in a San Francisco hospital room after having my aortic heart valve replaced by one made of a metal spring and some cow tissue (an ‘Edwards Sapien 3 Ultra’). I was glad to be alive, and I was clearly better off than my roommate, an elderly gentleman with a wrinkle-ridden oblong face and no visible hair. Heavily sedated and apparently dying from double pneumonia, he was a convenient roommate: no idle conversation, no moaning in pain, no shouting for nurses, no snoring, no watching late-night TV game-show reruns.
I don’t know what happened to my roommate – I escaped after two days. Back home, my healing went well, ‘for a person my age’, as the doctors routinely reminded me. But it was not entirely good news. My artificial heart valve – by decreasing my chances of dying from heart disease – has increased the likelihood of my dying from something worse (such as pancreatitis or a brain tumour).
Biophysicists have calculated that, with maximal improvement in health care, the biological clock for humans must stop between 120-150 years. Biotechnology firms such as Calico, Biosplice and Celgene are putting this to the test by scrambling to extend our normal lifespan as far as they can. However, a basic problem, at least thus far, is that a sustained quality of life has not been extended to keep up with our expanded longevity.
As people get older, they are not gaining economic security, maintaining their usual level of independence, extending their social relationships, or avoiding chronic illnesses. For instance, about 85 per cent of older adults in the United States have at least one common chronic illness such as diabetes, heart disease, arthritis or Alzheimer’s. Thus, many routine tasks such as bathing, making the bed, doing errands, shopping, picking up items off the floor, or walking without falling cannot be performed without help. In short, as we live longer we are also unwell for longer.
Psychological depression, caused by physical illness plus associated medical expenses, often contributes to even more decline. Almost every day a new ache or pain, of uncertain duration, pops up and adds to ongoing maladies. Undesirable, but necessary, medical compromises gradually squeeze the vitality out of a chronically ill person. In most cases, death is not a sudden event at the end of life (except as a legally defined physical state). Rather, it is a long process of progressive functional decline.
From my perspective, preventing death is not always more important than promoting the quality of life. What value is there in existing if the ability to do and experience what you most value becomes unavailable? It is, indeed, possible to live too long.
The philosopher Friedrich Nietzsche’s character Zarathustra commented that:
Many die too late and some die too early. Still the doctrine sounds strange: ‘Die at the right time.’ … Many too many live, and they hang on their branches much too long. I wish a storm would come and shake all this rottenness and worm-eatenness from the tree!
Nietzsche would have probably approved of the cult comedy-drama film Harold and Maude (1971), showing a timely and poignant death. Twenty-year-old Harold, bored and obsessed with suicidal thoughts, meets 79-year-old Maude at a stranger’s funeral service. Maude, who breaks many social taboos, teaches Harold to make life fun. A year later, she calmly arranges her own death. Harold is shocked into realising the value of present-moment awareness.
An unsuccessful suicide attempt can leave the person even worse off
Unfortunately the popular press is apparently not ready to discuss the ‘rottenness’ and ‘worm-eatenness’ of the elderly. Take the July 2022 issue of AARP magazine, which offered older women ‘10 Things That Always Make You Look Stylish’ such as bold red lipstick, which they claimed will ‘help dingy teeth appear whiter’. Or the May 2023 swimsuit issue of Sports Illustrated, which featured the 81-year-old business woman Martha Stewart demonstrating, they said, ‘ageless living’ and showing a bit of cleavage without ‘much airbrushing’. Perhaps she won a genetic lottery – most of the old people I know have saggy skin and poor posture. They are sexually unattractive. They are a hazard as drivers on the road, or even as pedestrians. They forget things. They are expensive to maintain. Rational and open discussion of death is rare, especially in a culture where a charge of microaggression or ageism has become an all-too-common threat.
A notable exception to the death-discussion taboo was an item in KFF Health News in June 2019 that reported on an 86-year-old woman arranging a secret off-campus meeting with nine other seniors (who slipped away from their fancy retirement community near Philadelphia) to discuss ‘rational suicide’. Seniors currently account for about 18 per cent of suicides in the US. An unsuccessful suicide attempt can leave the person even worse off. As one of the participants in the Philadelphia meeting put it: ‘We only get one crack at it. Everyone wants to know what to do.’
At present, medical personnel are left to deal with the toxic underbelly of a death-phobic culture. Only pain medication that may, as a side-effect of treatment, hasten death is a generally acceptable life-terminating procedure. As defined by the World Health Organization, palliative care improves the ongoing quality of life of patients with life-threatening illnesses. In contrast, where it is available, legally authorised medical aid in dying allows a physician to prescribe a lethal dose of a drug at the request of a patient who intends to end their life. In my opinion, such a prescription would at least give suffering patients a comforting option, even if they ultimately chose never to use the drug.
In the US, 10 states plus the District of Columbia presently allow medical aid in dying. Relevant laws typically specify that the patient must be a mentally capable adult within an estimated six months of dying, and be able to self-ingest the medication. The legislation also usually includes more than a dozen safeguards, such as affirmation from two physicians and two independent witnesses that the patient was not coerced.
Countries other than the US that allow medical aid in dying (as of 2023 that’s Austria, Australia, Belgium, Columbia, Germany, Luxembourg, Portugal, Spain, Switzerland, the Netherlands and New Zealand) have varying medico-legal requirements. For example, to prevent ‘suicide tourism’, Canada requires that a patient be a Canadian resident. Switzerland does not have that requirement. In her book In Love (2022), Amy Bloom details the voluntary death of her husband in Switzerland, where the patient does not need to be critically ill or within six months of death. Bloom’s husband had severe Alzheimer’s and she reportedly acted on his insistence that he would ‘rather die on my feet than live on my knees’.
Just as it is wrong to compel people to die, so it is wrong to compel people to live
Specific criteria and customary medical practice apparently have significant effects on patient utilisation of medical aid in dying. For example, according to a Canadian government report, 10,064 patients received medical assistance in dying during 2021. By contrast, in California, with a similar population of about 39 million residents, only 486 patients received medical assistance in dying during the same year. California law requires that the patient self-administer the drug, and that the patient be within six months of death. Canada does not require self-administration, and medical assistance is available if the patient’s medical condition is ‘grievous and irremediable’. Nonetheless, in both Canada and California statistics show that, consistently over several years, more than 80 per cent of the patients who used medical aid in dying had previously been in palliative care. The average age was 76 years, and more than 60 per cent had cancer. It seems younger, healthy people are not routinely exploiting the system.
Medical aid in dying and other practices pertinent to end-of-life care are surrounded by enigmatic and controversial issues involving religious beliefs and civil rights. Many people believe that life is sacred, and therefore the beginning and end should be left to divine intervention. The doctrine of the ‘sanctity of life’, commonly based on a theistic metaphysics, holds that killing oneself or others destroys the God-given intrinsic value of life. By contrast, a secular utilitarian view holds that there is a duty to ‘maximise happiness’ and therefore a moral obligation exists to end a life when it is characterised by indignity and suffering. Some moral philosophers argue that, just as it is wrong to compel people to die, so it is wrong to compel people to live under conditions they find intolerable.
I do not have the wisdom or inclination to solve such ethical complexities. I do, however, hope that the ‘right to die’ becomes a civil liberty issue in the way that daily living options have been expanded for marginalised ethnic groups, women and gender minorities.
A few months ago, in order to dissolve some blood clots, my cardiologist prescribed the blood thinner warfarin – the principal ingredient in rat poison. I assume that I will die, not by choice, but by the lethal default of accumulated peripheral decisions. So far, I have been fortunate. My body’s awkward way to the exit has not diminished the gratitude I feel for the many undeserved blessings I have received.