As far back as Anastasia can remember, her mind has been devoid of visual images. She can’t picture friends, objects, places or anything visual in her ‘mind’s eye’. When she was 32, she learned the formal word to describe this lack of internal visual imagery – aphantasia (a condition brought to the public’s attention by the neurologist and Psyche author Adam Zeman, and which is estimated to affect 3 per cent of people). Then one day, Anastasia ate psilocybin or ‘magic’ mushrooms and it altered the contents of her mind profoundly.
‘I found it incredible because it was the first time I had images in my mind, and I realised that you can play with images, zoom in, zoom out, break down colours,’ she told Kevin Rebecchi, a researcher at Université Lumière Lyon 2, in a recent case report he published as a preprint on PsyArXiv.
This isn’t the first time that psychedelic use has been linked to a change in a person’s ability to see mental images. In 2018, a different team of researchers reported a similar case: a man they referred to as ‘SE’, who had aphantasia (induced by a traumatic experience) but who regained mental imagery 30 minutes after taking the psychedelic ayahuasca.
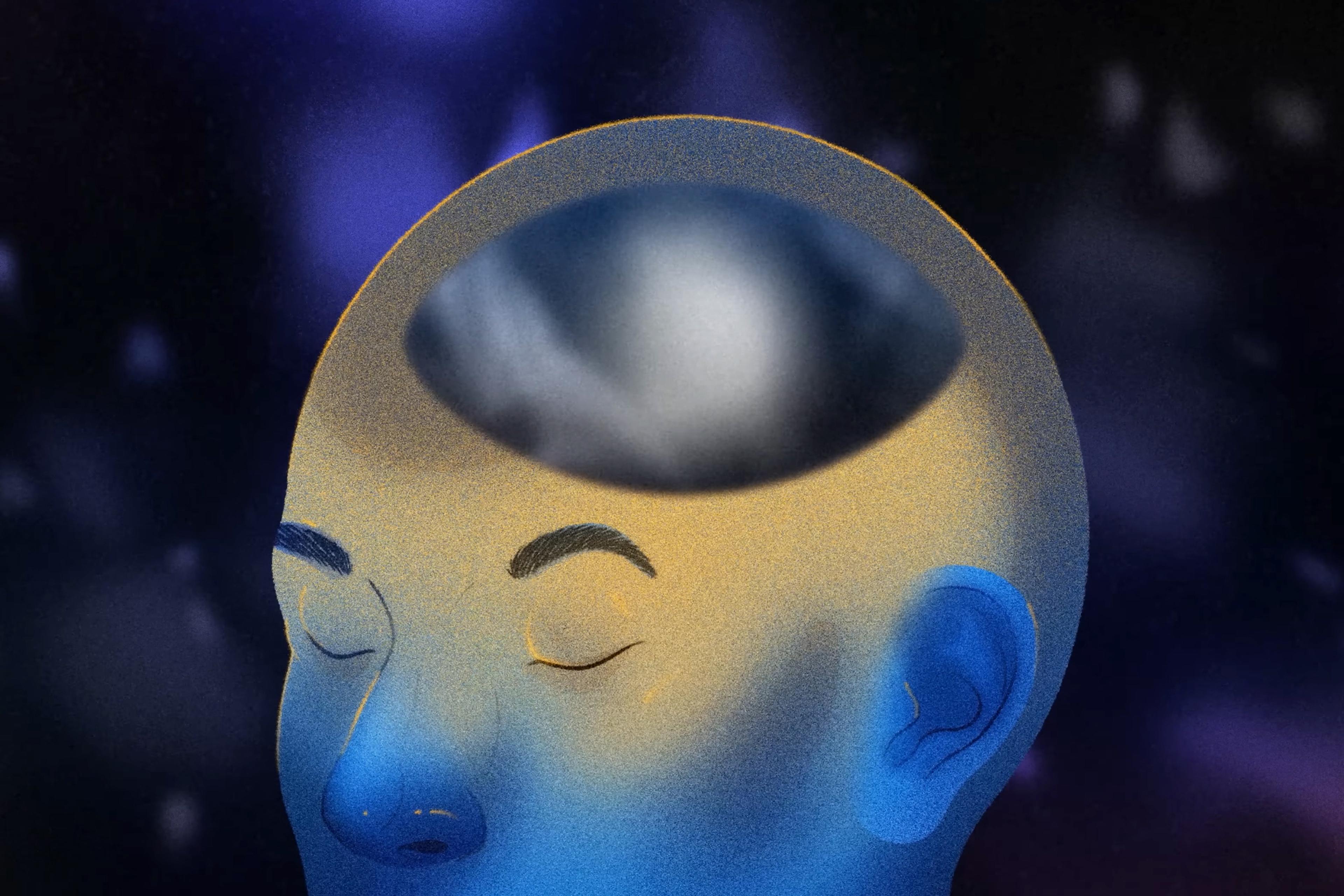
Joel Pearson, a psychologist and neuroscientist at the University of New South Wales who studies aphantasia, says that he’s been hearing anecdotal reports about psychedelics and gains in mental imagery for years. Psychedelics can increase neural connections in the brain, and these reports might be explained by an increase in neuroplasticity, Pearson says. It could also be that when a person has a brief experience of imagery during a psychedelic session, they learn what to look out for, which can drive their attention and amplify visual imagery in the weeks following.
But it’s unclear how common this phenomenon is. ‘What we don’t know is if you took 100 people [with aphantasia], put them through a [psychedelics] protocol, would one out of 100 get imagery?’ Pearson says. ‘Would 50? Ninety out of 100? We just have no idea. That being said, there seems to be something going on, and as a scientist that’s really interesting.’
Regaining mental imagery via psychedelics is certainly not guaranteed. In a reply to the case report on SE, David Luke, a psychologist at the University of Greenwich, presented a counter-example: a 39-year-old man, self-diagnosed with aphantasia, who reported smoking N,N-dimethyltryptamine (DMT – thought to be the imagery-inducing compound in ayahuasca) more than 1,000 times, yet he never experienced any mental imagery.
Case reports rely on their subjects to compare their ‘new’ level of mental imagery with their memory of how it used to be, so caution is needed in interpreting what’s going on with people like Anastasia and SE. Given the subjective nature of visual imagery, aphantasia is always difficult to measure. One issue with questionnaire methods (such as the Vividness of Visual Imagery Questionnaire) is that they might be affected by people’s differing awareness or interpretation of their own thoughts. It’s quite plausible that if you asked two people with the same level of imagery vividness to imagine a red apple, one could rate their mental image a 3, the other a 5 – even if they were actually visualising the exact same thing.
It is very curious that it seems to work for some people but not others, and I’m not sure why that is
This is why Pearson and others have been trying to introduce more objective measures for assessing aphantasia, such as looking at changes in pupil size when people are experiencing visual images. He hopes future studies that assess psychedelics and aphantasia will incorporate some of these tools.
‘I don’t think psychedelics are a magic cure for aphantasia and, in fact, it seems many people with aphantasia have used psychedelics without any imagery or visual experiences at all,’ says Reshanne Reeder, a cognitive neuroscientist at the University of Liverpool who studies mental imagery. ‘So it is very curious that it seems to work for some people but not others, and I’m not sure why that is – but the answer should be in the brain.’
People have been writing to Rebecchi to ask what kind of mushrooms Anastasia took, and how much – but these are questions he can’t (and won’t) answer. He’s not able to give out medical advice over the internet, but he also doesn’t think what happened to Anastasia can be applied more broadly.
In fact, it would be a mistake to assume that all, or even most, people with aphantasia would even want to deliberately introduce imagery into their minds – whether via psychedelics or other means.
In 2020, Pearson and his colleagues showed that brain stimulation could increase the vividness of mental imagery among neurotypical participants, but the effect didn’t last for long once the stimulation was over. If a study set out to give people imagery who had never experienced that before, Pearson says it would have to be done very carefully, because it’s unclear if it would be reversible. Moreover, he says that he has concerns about the ethics of giving people imagery who’ve never had imagery before.
‘Having strong imagery is much more associated with negative mental health,’ Pearson says. ‘Anxiety, hallucinations, PTSD, maladaptive daydreaming, cravings, addiction – a whole range of things cluster with strong imagery rather than aphantasia.’ He would prefer to start with people who had once had imagery and lost it, since they are more likely to have some memory of what it’s like.
There are certain memories – like from medical school – that she’s very glad never to revisit visually
Rebecchi has also heard from ‘aphants’ that his report makes them not want to take psychedelics because they don’t suddenly want to have mental imagery. ‘People told me: “OK, that’s very scary, I will never take them,”’ Rebecchi says. Research into psychedelic-assisted therapy is on the increase, together with more access to legal, guided psychedelic sessions in certain US states and other countries. In this context, the possibility that psychedelics could induce visual imagery in those who have never experienced it becomes an important concern related to informed consent.
‘If it turns out this is really a thing, then we need to add it to a long list of what may happen to you [when you take psychedelics],’ says Julie Holland, a psychopharmacologist and medical advisor for the Multidisciplinary Association for Psychedelic Studies (MAPS), an organisation submitting data to the US Food and Drug Administration for approval of MDMA-assisted therapy. ‘I don’t want my brain to change,’ she adds. Holland has aphantasia, and tells me there are certain memories – like from medical school – that she’s very glad never to revisit visually.
Rebecchi’s other work is focused on cognitive and neurodiversity; he doesn’t view aphantasia as a disorder that has to be fixed. One news article headline described what happened to Anastasia as her being ‘cured’ of a rare condition. Aphants do show some differences in visual working memory, visualising the future, and dreaming, but for many people with congenital aphantasia, they’re unaware that they have it because it’s not a hindrance to everyday functioning.
‘I think it’s important and interesting to make people realise that there are other possible life experiences, and just because we are made to believe that something is missing, doesn’t mean we are deprived,’ Anastasia told Rebecchi. ‘We simply do things differently.’