In the past 10 years, a quiet revolution has happened in medicine. From the United States to Scandinavia, health organisations are opening up their clinical records to patients. Not just test and lab results, but the very words that doctors write about individuals and their conditions. These ‘narrative reports’ were once considered the private possession of health professionals, to be kept away from patients’ prying eyes. Now, patients have been given the legal right to go online and take a look for themselves. Just like with online banking – via smart phones, tablets and laptops – patients can log in to online portals at their own leisure and access information about their medications, test results and referrals, as well as see their doctors’ own notes.
This openness seems like a good thing: from strep throat to cancer care, accessing health information can empower patients. But this might not be the case across all areas of medicine. When the problem relates to mental health, might too much transparency be a bad thing?
If you ask patients themselves, they are overwhelmingly positive about seeing their notes. Across physical and mental health, extensive surveys in Sweden and the US show that the vast majority of patients (96-98 per cent) who have accessed their notes believe it’s a good idea. Most view the practice as ‘very important’ for taking care of their health, and better remembering their care plans, such as why a medication has been prescribed and how often to take it. A 2018 study in the US compared the experiences of primary care patients with and without mental health diagnoses, and found that they were both similarly positive about open notes.
Initial evidence from more specialised mental health services – typically psychiatrists, clinical psychologists or psychotherapists – is also promising. A study at an outpatient psychiatry centre in Boston found that, after 20 months of open notes, patients reported better understanding of their mental health condition, increased recall about their care plan, and more knowledge about the potential side-effects of their medications. In Canada, patients with complex and serious mental health needs experienced increased progress in their care, greater engagement with treatment, and an enhanced sense of autonomy when given access to their notes.
Similar findings have been reported in psychotherapy. In a recent study, also in Boston, the majority of clients who were able to read their therapists’ notes online reported that access was ‘very important’ for feeling in control of their care, for understanding the psychotherapy process, and for trusting their therapist. Patients described reading their notes as strengthening their alliance with mental health clinicians; their comments included: ‘It was confirming. It helped me to understand my situation’; ‘It validates my thoughts in writing’; and ‘I felt that my therapist was really listening to me.’
However, not all patients are happy. Across mental and physical health, a small minority (between 3-5 per cent) in the same study described being very confused or more worried after reading what their doctor, or other clinicians, wrote about them. Some psychotherapy patients felt offended or upset by what they’d read, or reported inaccuracies in their notes. As one patient attested: ‘[Th]e note seemed judgmental in a negative way. After reading it, I felt badly, like she didn’t like me as much as I had thought.’ Others reported incongruencies between what they read and what was conveyed in sessions: ‘[S]he told me one thing yet I read something else in the note. I don’t know that I would see her again due to this.’ In such instances, trust in mental health professionals can become strained. And given that psychotherapy drop-out rates are as high as 20 per cent, changes that risk treatment abandonment are troubling.
Such cases present a dilemma for clinicians. In general, doctors’ initial concerns about note-transparency generating extra email traffic, office visits and complaints have not been borne out. The majority of primary care clinicians are positive about the experience, reporting no major workplace burdens. But when it comes to mental health care, psychiatrists and clinical psychologists remain cautious. In the US, half of clinicians with the Department of Veterans Affairs (VA) – the nationwide health system that provides all enrolled veterans with access to their mental health notes – said that they’d be ‘pleased’ if open notes were discontinued. Nearly two in three clinical psychologists and a third of psychiatrists in Sweden reported being less candid in their notes as a result of the practice. This is an issue because it might mean notes are inaccurate, or that an incomplete picture about the patient is shared with colleagues, for the sake of not causing offence or damaging the relationship. Notes that place a premium on pleasing patients might inadvertently result in errors, or in compromised levels of care.
For some mental health patients, full transparency might not be appropriate or helpful. Consider for example, a patient with borderline personality disorder – an illness characterised by extreme mood swings, self-destructive behaviour and unstable relationships. Some patients with this condition might become so deeply upset by what they read that it leads them to emotional harm or self-injury. In these cases, keeping notes private might be better for both the patient and the clinician.
Doctors have contractual obligations: a duty to ‘first do no harm’, and to prioritise the wellbeing and interests of their patients. They are also duty-bound to respect patients’ autonomy: to give us accurate information about our health, and the space and time to make our own medical decisions. Opening mental health notes therefore presents a dilemma: how should doctors balance honesty and openness with the possibility of harm to patients?
Some services have attempted to resolve this by prohibiting any patient with mental health problems from accessing clinicians’ notes. For example, only 11 out of 21 of Sweden’s regions offer open notes to mental health patients. But this blanket approach means many potential benefits might be lost. In the US, psychotherapists are not obliged to share their notes with patients – the new federal ruling specifically exempts health professionals from sharing clinical notes if doing so will cause harm. This could include the worries around mistrust and disengagement given above – but this discretion could be misused. Allowing doctors to decide when to share notes on a case-by-case basis could shift medical communication back to a model of problematic power imbalance.
So, should mental health notes be opened or closed? In complex cases – and pending further research – sharing mental health notes might prove riskier for some patients or conditions. Yet, exclusively denying access to this diverse and vulnerable patient population could also result in greater harms from stigmatisation. Perhaps the prudent response, while we await further evidence, is the call to reimagine clinical notes: not just as a record for clinicians, but as a communication tool with patients.
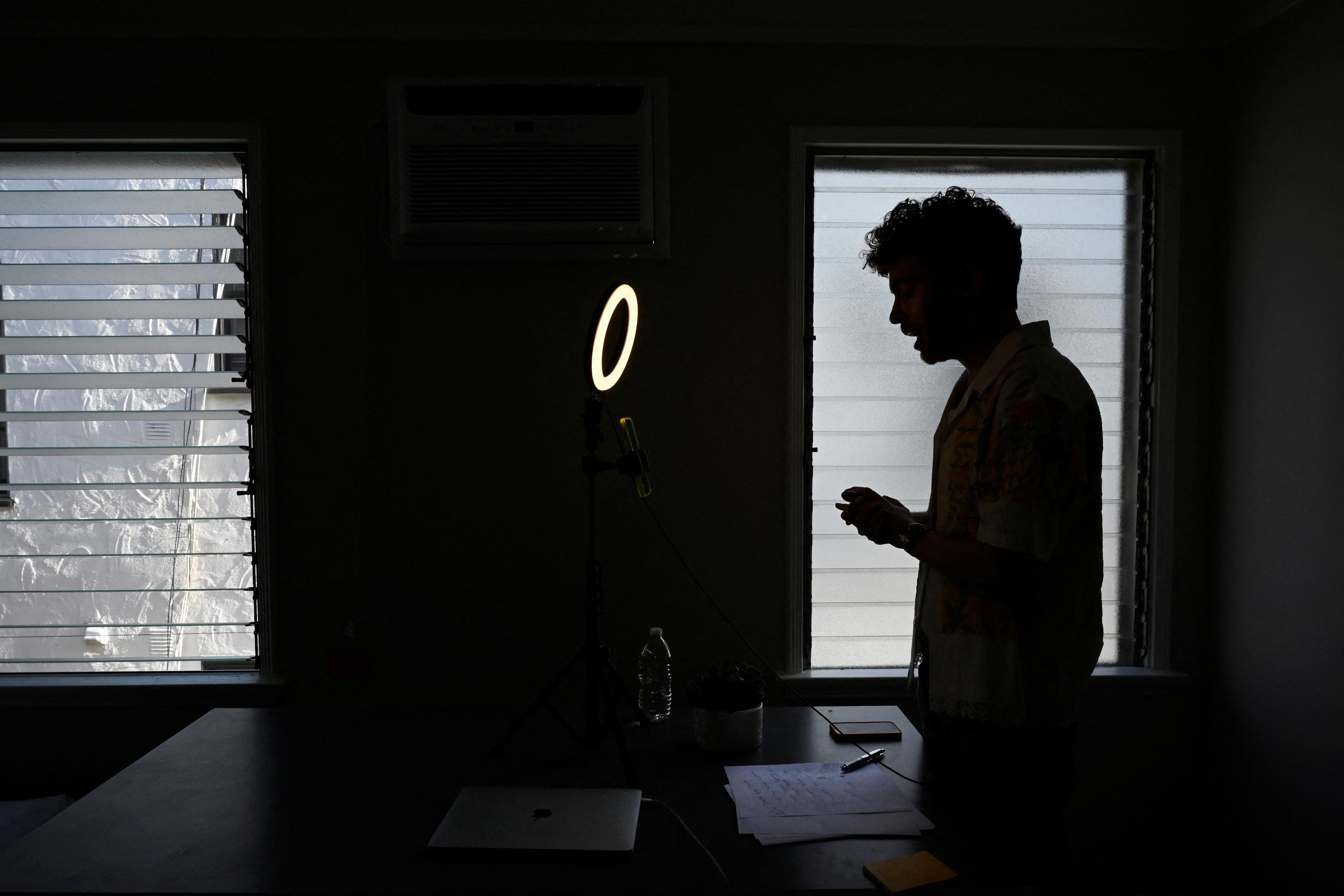
Health professionals, who are used to writing just for themselves and their colleagues, will need training in how to communicate accurate, clear and empathic notes to their patients. Dependent on the individual’s diagnosis and presentation, the tone of notes might need to be carefully crafted to provide patients with encouragement, open dialogue and support. Recent successes with a web-based course in the US suggest that this is achievable. Patients will need guidance too. With notes conceived as an online extension of the appointment, patients can be taught the benefits and risks of choosing to access their notes, and about how to address concerns with clinicians.
Culture change in mental health care is not easy, and innovation inevitably invites both benefits and challenges. For many patients, access to notes can be hugely helpful, reducing stigma and improving care. In the new era of transparency, clinicians must adapt. And by treating patients like care partners, health professionals might find themselves empowered too.