Rachel gets out of bed slowly, very slowly, still troubled by the oppressive weight of depression that she has been carrying for the past six months. This, despite the therapist she sees, and despite the antidepressant pills she has been taking, seemingly forever. However, her treatment today is different. Instead of taking a pill, she puts a cap on her head – a futuristic-looking device containing electrodes that both read her brainwaves and pass a gentle electrical current across her scalp. She boots up her iPad and enjoys the distraction of a game while receiving her treatment: electrical stimulation to her brain that is driven and refined by ongoing recording of her neural activity. At the end, she rates how she is feeling. This and other data from her session, and her previous treatments, is fed into an algorithm that continually refines her ongoing course of treatment.
This might sound far-fetched, but is far from it. Beyond recognising and addressing the importance of social interventions to ameliorate the external conditions that can contribute to mental health problems, the treatment of depression is currently evolving in unexpected ways. This is based on a shift away from thinking about depression as a disorder of ‘chemicals in the brain’ to an understanding that depression is underpinned by changes in electrical activity and communication between brain regions.
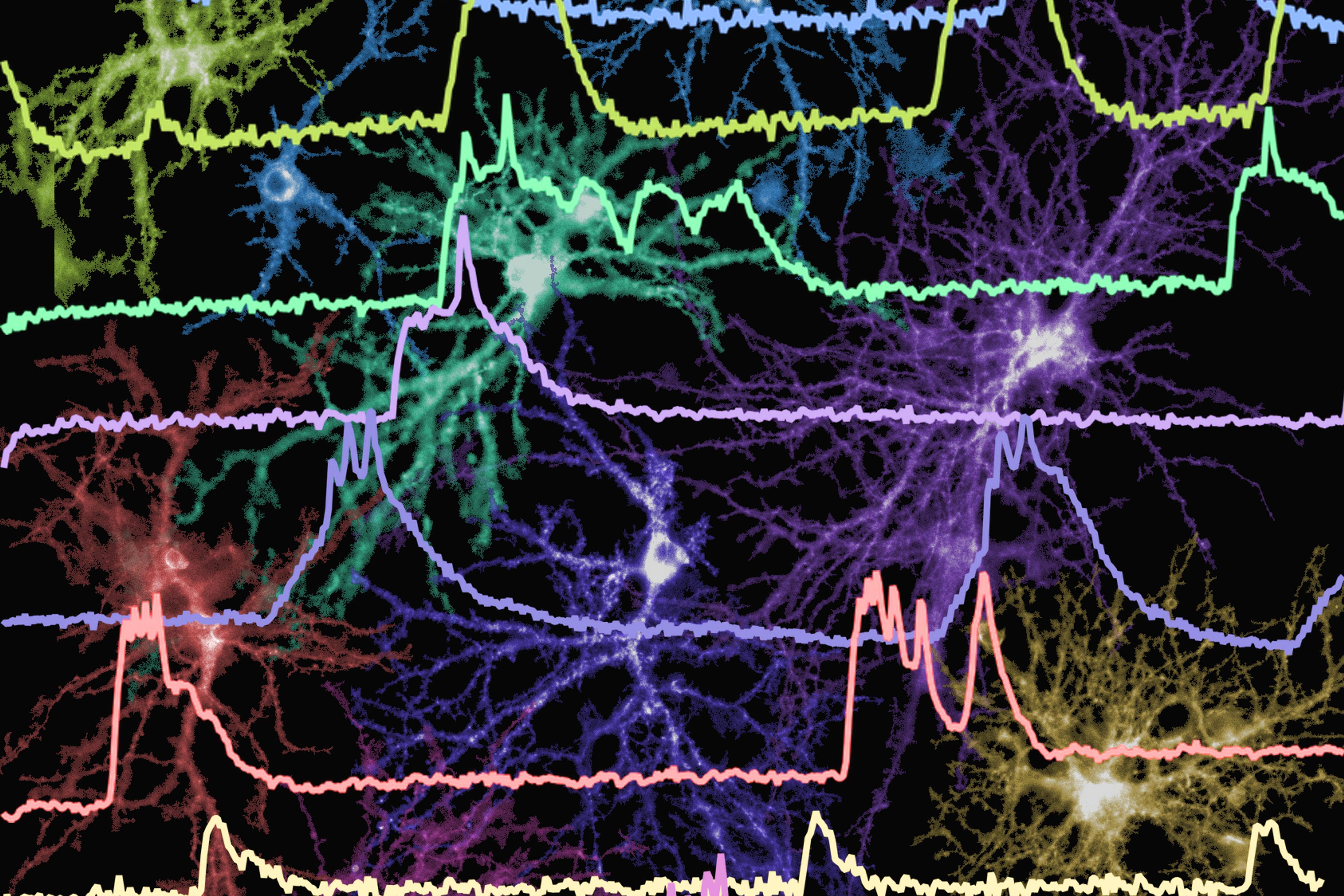
Brain areas talk to one another by firing in rhythm together, at specific frequencies, forming complex networks that underpin important brain functions. For example, nerve cells in frontal and parietal areas of the brain oscillate in rhythm together (usually between 4 and 8 times per second) while we are actively trying to remember something. There is increasing evidence that depression is associated with changes in several of these networks, particularly those that connect multiple brain regions at long distance. One knock-on consequence is the overactivity of some parts of the brain and the underactivity of others.
Unbeknown to most of the public, there’s a new therapy, now established in clinical practice, called transcranial magnetic stimulation (TMS) that can address some of these brain-based changes seen in depression. In TMS, a figure-8-shaped coil held over the head generates a magnetic field that stimulates localised brain activity and the strength of connections between multiple brain regions. To treat depression, the TMS pulses are usually targeted to the front of the left side of the brain, a region that is consistently underactive in patients with depression. Although several decades of clinical trials have established the effectiveness and safety of TMS, especially for patients who have not responded to standard antidepressant medication, an ongoing challenge is that it is time-consuming and inconvenient. Patients must attend a clinical setting on a daily basis, five days per week, for up to 6 weeks.
For this reason, efforts are underway to develop alternative forms of brain-stimulation treatment that could be administered in a patient’s home. Of these, the research is most advanced for transcranial direct-current stimulation (tDCS), a surprisingly simple process, the ideas behind which are not new. People have experimented with the use of electrical currents to change brain activity since Scribonius Largus, physician to the emperor Claudius, applied a type of electric ray to the brain during the time of the Roman Empire.
Unlike TMS, tDCS doesn’t directly stimulate the nerve cells of the brain, but subtly shifts the likelihood that they will fire in the future. A weak electrical current passes in one direction between two electrodes held in sponges placed on the scalp. This produces changes in brain activity beneath the electrodes and, when applied repeatedly to an appropriate area of the brain, such as left frontal regions, there is evidence from more than 10 clinical trials that it can help patients with depression. The development of tDCS in depression is at an earlier stage than TMS, but it is progressing rapidly, especially since its simplicity makes it viable as a widespread home-based therapy.
On that front, in recent years, interest has also grown in a related but distinct form of electrical stimulation – transcranial alternating-current stimulation (tACS), which differs from tDCS in that the applied electrical current passes back and forth between the electrodes in an alternating manner, rather than in a single direction. Likely working through a different mechanism than tDCS, via entrainment, tACS is applied at a specific frequency – the rate at which the current passes back and forth between the two electrodes – and this is used to increase or ‘entrain’ the firing of the targeted neurons at that frequency. One hypothesis is that depression is associated with a miscommunication between the two sides of the front of the brain at the alpha frequency (between 8 and 12 Hz); if so, tACS could help address this via entraining firing of these alpha-frequency-based connections, thereby strengthening communication within the networks, or even by slowly adjusting the alpha frequency itself, if faster or slower firing of these networks were found to result in therapeutic benefit.
A key advantage of tACS is its potential for being personalised to each patient. To understand this, it is important to note that everyone has an ‘individual alpha frequency’, which can be measured with electroencephalography (EEG). It is the specific frequency at which their neurons will fire when they are in a relevant mental state, such as while resting and mind wandering. For instance, this might be 8.8 Hz for me, and 10.2 Hz for you. Crucially, entrainment via tACS is much more likely to occur if stimulation is applied at a personalised frequency close to a person’s existing individual frequency.
This personalised approach is something that my colleagues and I are already starting to test. When we evaluate patients with depression for the use of tACS stimulation, we’ll have them undertake an EEG so that we can tailor the stimulation to their individual alpha oscillation frequency. And this is where I think things start to get really interesting. What if, instead of measuring their brain oscillations once in the clinic, we could measure them every day at home before, after, and maybe even during the treatment itself? And what if that ongoing reassessment of their brain activity could be used to update their stimulation parameters – creating a closed-loop treatment system?
My team believes that all this could happen, and we’re working on a device that patients could wear at home in real time. Moreover, we’re exploring not only the capacity for continued updating of the stimulation parameters on the device, but also ways to enhance this via cloud-based artificial intelligence processes that continually monitor outcomes and compare these with efficacy data from previous patients, creating a flexible system that becomes progressively more effective.
This is the futuristic, yet increasingly plausible, scenario I painted for Rachel at the beginning of this essay. Our ambition is for an advanced form of treatment that could potentially revolutionise the way patients with depression are managed. How close are we? At this stage, there is only limited evidence that tACS is therapeutically helpful, and the advanced closed-loop system I described has not been clinically tested yet. However, early studies have indicated that simpler forms of tACS can be used to treat depression, and we are making rapid progress in developing the technology to allow us to conduct at-home trials. Unfortunately, to make the scene with Rachel a reality, I fear that, as well as overcoming clinical challenges, we will also have to face up to some of the same cultural hurdles that have beset TMS in recent years.
Psychiatry is, at heart, a conservative profession containing within it many clinicians who have worked with one of the existing forms of treatment – medication or psychotherapy – for many years. Although many have been open to understanding the evidence for a new treatment such as TMS, and integrating it into their therapeutic practice where appropriate, there has also been considerable pushback from some within the profession. Despite three decades of research establishing its efficacy, there have been articles in psychiatric journals repeatedly questioning the value of TMS, but without really addressing the science supporting its use. What’s more, its use was also sidelined in the recent clinical practice guidelines for mood disorders from the Royal Australian and New Zealand College of Psychiatrists – and that’s despite advocacy from the experts within the college to ensure its appropriate representation.
At times, this resistance seems to reflect a perhaps wilful ignorance of evidence or even an ideological approach to medicine rather than an evidence-based one. There is a danger that a highly novel treatment, such as home-based closed-loop stimulation, will produce a similar degree of professional resistance, especially given that treatment informed by artificial intelligence could be seen to reduce the role of the clinician in the decision-making process.
Despite these challenges, my research group and many others in the field are pushing ahead to develop new and innovative treatments. We’re motivated to overcome the challenges many of our patients face with the therapies currently on offer. The next steps are to conduct substantial clinical trials to convince clinicians and regulators alike, and we also need to meaningfully engage people with lived experience of depression, to ensure these home-based brain-stimulation devices are acceptable and accessible. Existing depression treatments, such as medications and forms of psychotherapy, are only moderately effective. I’m hopeful that soon there will be a new, convenient and personalised option that will have a meaningful impact on what many are calling the mental health crisis.