Almost everyone reading this article will know someone with a mental health disorder, even if they are lucky enough not to have experienced one themselves. Unfortunately, although many treatments are available today, they continue to involve a great deal of guesswork. For instance, if someone is feeling down and sad every day or has lost all interest in the things they usually like (the symptoms of major depression), their GP will usually either offer them an antidepressant drug or put them on a waiting list for psychological therapy. These treatments are somewhat effective: each treats depression successfully in about half of cases. The problem is, there is currently no way to tell whether someone would be more likely to get better after therapy or after drugs (or a combination of the two). Instead, clinicians use trial and error.
To better predict who needs which treatment, we need to understand how and why mental health treatments work – moreover, we need to find out why, for too many people, they don’t work at all.
I come at this dilemma as a neuroscientist. An essential but unanswered question in my field is: can the brain changes evoked by treatments – whether drug-based or psychotherapy – explain why only some people get better after each specific form of treatment? Perhaps you are surprised or sceptical that neuroscience would have anything to say about the effectiveness of psychotherapy. My answer to this is that both medication and psychological therapy are biological interventions – many studies show that both change the biology of the brain. This shouldn’t really be a controversial statement, but it is. Within psychology, there is a raging debate over whether or not mental health disorders are also ‘brain disorders’.
The default answer on many medical websites is ‘Yes’ – although this is often ascribed to a simplistic view that mental health disorders are caused by chemical deficits in the brain (this explanation is far too simplistic – it depends on the region of the brain, the specific group of patients, and many other factors). On the other hand, a growing chorus of psychologists and philosophers think that mental health disorders are definitely not brain disorders. For instance, a report published by the British Psychological Society’s Division of Clinical Psychology in 2016 claimed: ‘There is no firm evidence that mental distress is primarily caused by biochemical imbalances, genes, or something going wrong in the brain …’ Rather, the authors suggested that the cause of mental distress is outside the body: external environmental factors, such as difficult childhood experiences, abuse or poverty. This goes hand in hand with assertions that treatment, too, should come from outside the body: psychological therapy, as well as political and societal change.
I agree that there is no doubt that external factors are extremely important risks for mental health disorders, and I do not doubt the utility of psychological or social interventions. I suspect the heart of the disagreement originates from people’s vastly different ideas of what it means to say that something is a ‘brain disorder’.
Think about another organ system: the heart. If cardiovascular dysfunction arises after a lifetime of environmental risk factors (diet, stress, smoking) does that mean the condition is not really a ‘heart disease’? In such a case, should research and treatment for cardiovascular dysfunction primarily (or exclusively) focus on preventative diet and lifestyle interventions, rather than on the biology of the heart? Few people would go so far. Instead, they’d probably agree that while the external factors clearly made an important contribution to the disease, nonetheless the biology of the heart remains crucial to understanding and treating the disease.
I believe the same logic applies to mental health conditions, including those with important environmental risk factors, such as post-traumatic stress disorder, which by definition requires a preceding (external) trauma. How does trauma cause post-traumatic stress disorder? Just as smoking, stress or diet affect the biology of the heart, trauma changes the biological workings of the nervous system. In turn, these neural changes alter our thoughts, feelings and behaviours. If someone has particular brain characteristics that make them vulnerable (these could also originate from environmental or genetic sources), such neural changes can result in post-traumatic stress disorder (PTSD). (I should add that I do not think mental health occurs only via the brain – the rest of the body also plays a crucial role.)
In the past 20 years, neuroscientists have made huge leaps in identifying brain changes in people suffering from mental health conditions, including depression, anxiety disorders, PTSD and psychosis. Each leap has been accompanied by a great hope that this finding would be the crucial variable for improving mental health treatment. Occasionally, this hope has been justified. For instance, in 2008, some patients with encephalitis who were experiencing delusions, hallucinations and other symptoms were found to produce autoantibodies that target particular receptors in the brain (most commonly, the NMDA receptor). These patients are normally first seen by psychiatrists, given the similarity of many of their symptoms to classic psychosis. Now, patients with similar symptoms can be screened to search for particular antibodies in their blood or cerebrospinal fluid, and, if the search is positive, treated using immunotherapy.
However, aside from such rare exceptions, understanding how the brain’s circuitry changes in mental health conditions has not yet revolutionised our ability to treat mental health disorders. Part of the reason is that we are only just beginning to learn how existing treatments, such as antidepressant medication and cognitive therapy, change the brain.
A key question here is whether antidepressant medication and psychological therapy cause similar changes in the brain. If they do, this would imply that, although it might feel different to take a medication compared with attending therapy sessions, the two treatments are working in similar ways, on similar neural processes. On the other hand, if each treatment did different things to your brain, this would indicate that they work via different neural mechanisms, with important implications for potential treatment effectiveness.
To find some answers, my colleagues and I at the MRC Cognition and Brain Sciences Unit at the University of Cambridge recently gathered data from 24 previous antidepressant trials and 19 previous cognitive therapy trials, thanks to scientists around the world who sent me their data. This included brain scan data from hundreds of patients with different disorders (depression, social anxiety and several others). By comparing changes in brain activation after a treatment compared with pretreatment, we were able to visualise which bits of the brain changed as a result of each treatment, and look for any areas of overlap.
The results were striking – there was no overlap between the brain changes from antidepressant medication and those from psychological therapy. Instead, psychological therapy specifically changed brain activation in the medial prefrontal cortex, a region involved in attention and awareness of your emotional state, whereas antidepressant medication specifically changed activation in the amygdala, which is more directly implicated in generating emotional states.
Although medication and therapy affected anatomically distinct regions, these regions are functionally related. In a separate analysis involving data from a large group of participants exposed to emotional stimuli in a brain scanner, we found that both regions significantly overlapped with the brain’s so-called ‘affect network’. This network is made up of interconnected regions in the brain that work together during various emotional or feeling states (angry, happy, sad, and so on). In other words, antidepressant medication and psychological therapy act on different parts of the same functional brain network (see image below).
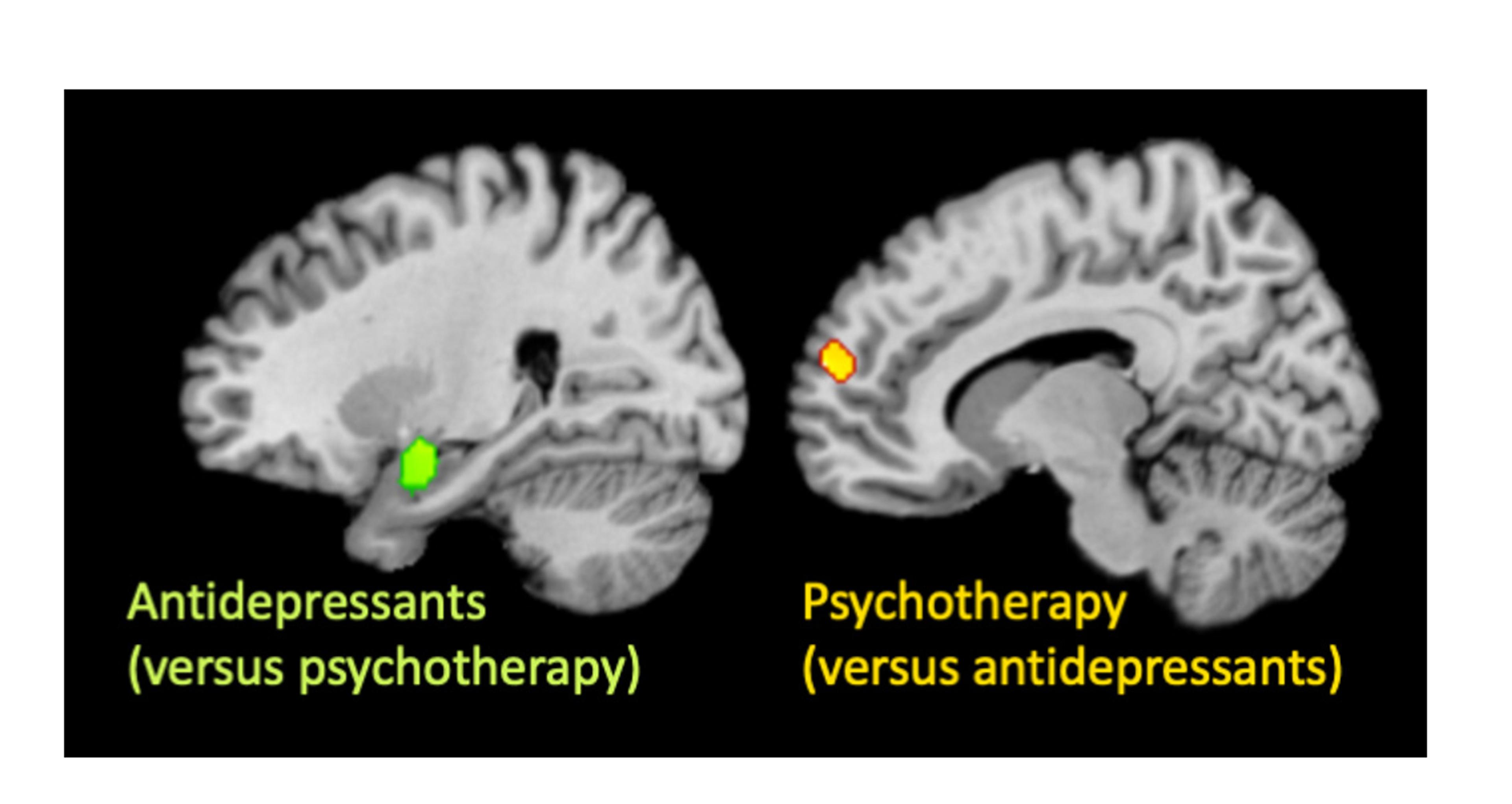
Antidepressants, but not psychological therapy, changed activity in the amygdala (green, left), while psychological therapy, but not antidepressants, changed activity in the medial prefrontal cortex (orange, right). Image supplied by the author
Based on what’s known about the different components of the affect network, our work suggests that psychological therapy alters the functioning of brain regions involved in focusing your conscious attention on feelings, which makes sense given the aims of many types of therapy. By contrast, antidepressant medication changes a region of the brain involved in experiencing feelings themselves – potentially directly changing your emotional experience. These findings have important implications for treatment, implying that the two treatment modalities could work additively; that is, they could be more effective in combination (supporting this, other work has shown that medication and psychological therapy treat depression better in combination than alone).
Another important implication of this line of work is in showing the potential value of discovering ‘biomarkers’ or brain signatures that might predict which treatment is best for which patient. After all, if antidepressant medication and psychological therapy have distinct effects on the brain, then patients whose brains show specific localised functional changes (say, in the medial prefrontal cortex) might be more likely to respond to the interventions that target those same regions (from our study, you might hypothesise that these people would respond better to psychological therapy). In contrast, those with changes elsewhere (such as the amygdala) might be more likely to respond to treatments that target the amygdala (ie, antidepressant medication). Of course, we need to test these hypotheses, but already previous research studies support the logic, showing that different treatments work better for patients with particular brain activation patterns.
A brain-based approach to mental health disorders might also help us invent new treatments. During my PhD at University College London, I ran a trial of brain stimulation in depression with the neuroscientists Jonathan Roiser, D Chamith Halahakoon and a team of NHS clinical psychologists. We visited NHS Improving Access to Psychological Therapies (IAPT) clinics in London, scanned patients’ brains, then gave them brain stimulation (tDCS) immediately prior to their psychological therapy sessions, and then scanned their brains again when treatment was complete. When I was recruiting patients for the trial, I heard so many tales about treatment failures: patients who had tried everything before, and nothing worked. I would love to say that our trial was the exception to this rule, that we discovered a way to massively increase the number of patients who recovered after a course of CBT (as we’d hoped). We didn’t manage that, but we did make an exciting and important finding.
Some patients showed a significant benefit of the combined treatment, and some did not – just like in so many treatments for depression. Crucially, the brain scans we conducted showed that it was the patients with the highest pretreatment activity in the prefrontal cortex (the brain region targeted by the brain stimulation and which has been shown to be disrupted in many patients with depression) who were the ones most likely to respond to treatment. This wasn’t the case for a placebo comparison group, who also received therapy – in other words, increased activation in the prefrontal cortex was a specific predictor or biomarker that predicted the likely effectiveness of the combined treatment. Although this was several years ago, it remains my favourite result from all my research. Despite a not particularly successful treatment overall, we uncovered useful information about who it worked for – and why – potentially taking us one step closer to identifying the right treatment for each patient.
The most vital quandary of mental health disorders today is not whether they change the brain but how. A cleverer approach to treatment in future might measure a patient’s brain changes, or use a smartphone app to quantify key aspects of behaviour, and direct each patient to the treatments that work best for those brain or behavioural metrics, irrespective of their diagnosis. Some studies have begun to test this, but we are a long way from a solution. A crucial scientific challenge of our era will be measuring the cognitive and biological changes occurring in mental health on an individual level, and mapping out their relationships with treatment outcomes. It will not be easy, but it could be transformative for mental health. I’m hopeful that a more personalised approach, driven by scientific data and theory (including neuroscience findings), could eventually improve the lives of people with mental health disorders by helping clinicians find the right treatment for the right patient – whether that treatment is medication, therapy – or something completely different.








