Psychiatry views the common mental afflictions of depression and anxiety as illnesses. From our perspective as biological anthropologists, we believe this is a colossal error. Researchers in our field are trained to think about humans in the same way that we think about chimpanzees, macaques and any other animal on the planet. We recognise that humans, like all other species, evolved in environments that posed many challenges, such as predation, starvation and disease. As such, human psychology is well-adapted to meet these challenges. Yet psychiatry has largely ignored the implications of human evolution for mental health (there is a subdiscipline of ‘evolutionary psychiatry’ but it has limited influence).
Over time, species have adapted to their environments via the process of natural selection. Any random genetic mutations that had bodily or psychological effects that increased an individual’s chances of reproducing were more likely to be passed on, and to increase in frequency across successive generations. The genes we’re talking about produced (in concert with other genes) complex adaptations for reproduction, not necessarily for increased chance of survival or wellbeing. A genetic mutation that increased an individual’s tendency to experience bliss, and not to worry about enemies, wouldn’t have lasted for long in the gene pool. We believe this unceasing process has many ramifications for mental health research.
First, evolution has not shaped humans to be perpetually happy or free of pain. On the contrary, we’ve evolved pain neural circuits because our ancestors who experienced physical pain in response to environmental threats were better able to escape or mitigate those threats, out-reproducing their peers who didn’t experience pain. We evolved to experience suffering as much as we evolved to experience wellbeing.
Second, fellow members of one’s species are often fierce competitors for food and mates, and transmitters of disease. To avoid competitors, many species, including 70 per cent of mammalian species, are solitary. But most primate species, including humans, live in groups. The benefits of cooperating in defence against predators have outweighed the costs of group living, including social conflict. These social conflicts are the source of much human emotional suffering or what psychiatry frequently views as common mental disorder.
Third, evolution has shaped the primate life course into distinct phases, and recognising these has implications for understanding different manifestations of mental disorder and strife. To simplify matters, the ‘juvenile phase’ involves rapid growth of the body and brain. During this phase, mothers provide food and protection while juveniles acquire information about their ecological and social environments. As individuals reach adult body size, they then undergo a profound physiological and neurological transition to a ‘reproductive adult’ phase. Finally, after reaching the adult reproductive phase, the body, including the brain, begins to senesce – to age. Even an individual who has transitioned to the adult reproductive phase and has managed to avoid predators, pathogens and starvation will eventually succumb to the failure of some critical organ or other.
All disorders, including mental disorders in psychiatry, are caused either by genetic mutations, failures of physiological functions due to ageing, and/or environmental factors – the relative risk of each causal factor varies across the different life phases. Disorders caused by genetic mutations will by their nature tend to be highly heritable, yet if they are harmful to reproductive success, we would predict that they will also be relatively rare in early life because natural selection will have eliminated them over time. Disorders caused by senescence should obviously be rare at younger ages but common at older ages, and might also be highly heritable. Finally, disorders caused by common environmental factors, such as germs, toxins or injuries, should be relatively common across the life course, but not be highly heritable. Likewise, conditions such as physical or emotional pain that are defences against environmental challenges, should be common across the life course, and not highly heritable.
To test the logic of this approach we used data from a recent large study from the Brainstorm Consortium with more than a million participants to categorise common disorders by their age of onset, prevalence and heritability. Disorders such as Alzheimer’s and Parkinson’s disease (in brown in Figure 1 below), usually categorised as ‘neurological’ rather than ‘mental’ disorders, are overwhelmingly more prevalent in older adults (among whom they are relatively common), and thus probably due to senescence. Schizophrenia, bipolar and autism (in red, Fig 1), on the other hand, are relatively rare, highly heritable, and typically onset during the juvenile or early adult phases, suggesting that they are caused by mutations in the genes regulating development.
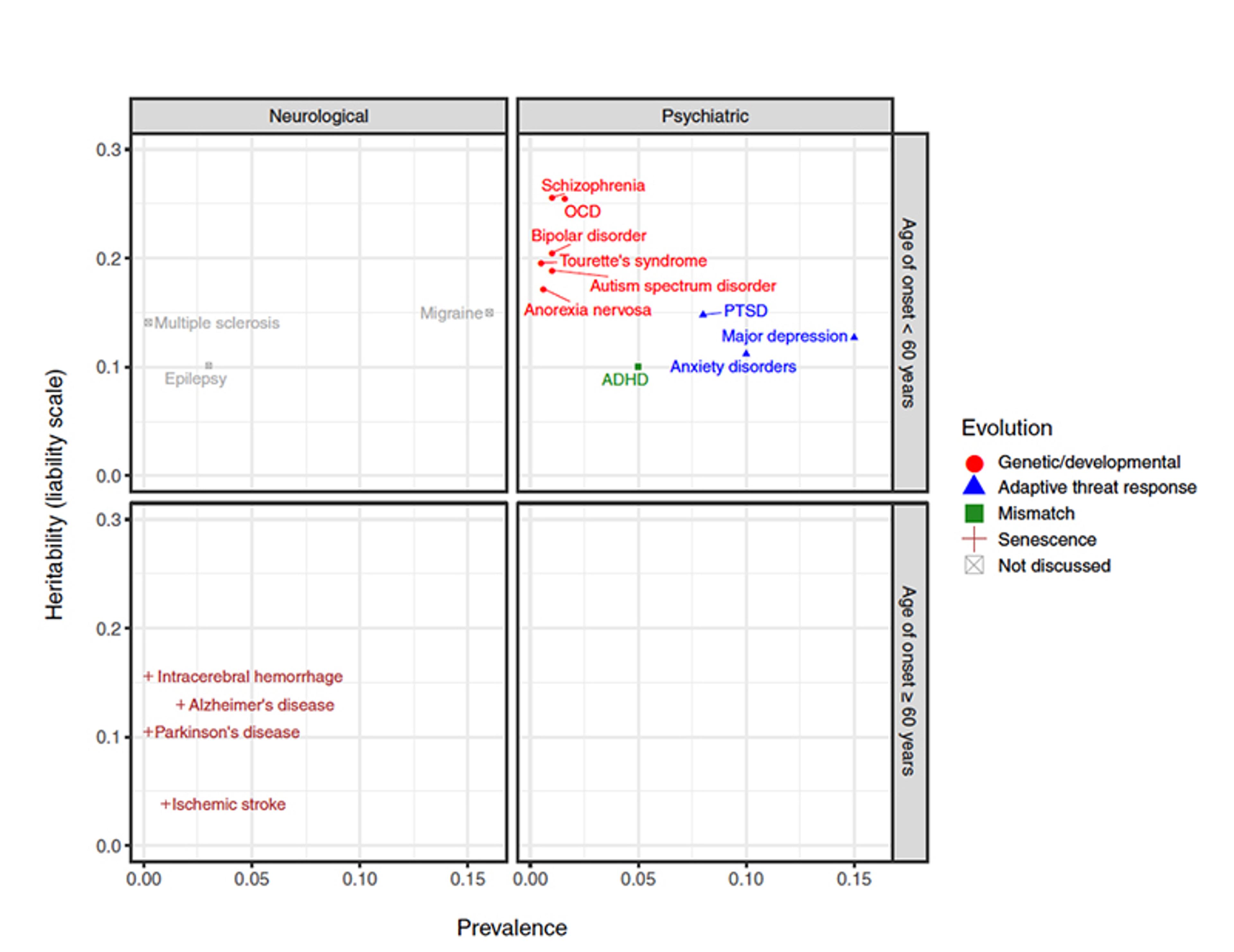
Figure 1: Mental health conditions by their prevalence, heritability, and age of onset. Figure from Syme and Hagen (2020)
Finally – and most importantly for our argument – conditions such as depression, anxiety and post-traumatic stress disorder (PTSD; in blue, Fig 1) and attention deficit and hyperactivity disorder (ADHD; in green, Fig 1; not discussed here), are in contrast relatively common throughout the life course. In fact, depression and anxiety are the leading contributors to the burden of mental health problems (see Figure 2 below). They also have low heritability and can onset at any age. This suggests that these afflictions are caused, in large part, by common environmental factors – perhaps the social conflicts that have been endemic through our species’ evolutionary history.
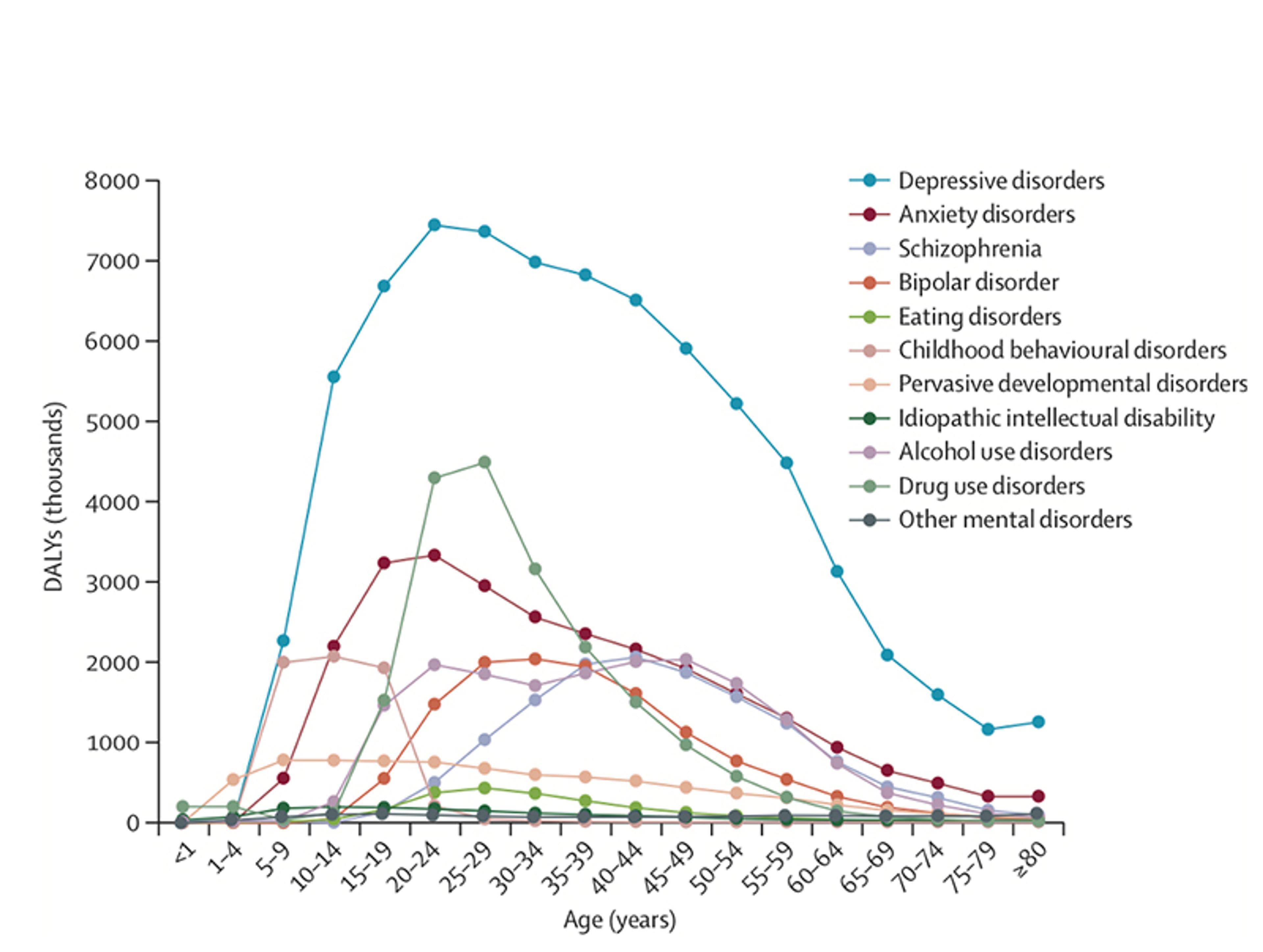
Figure 2: The global disability-adjusted life years (DALYs) imposed by mental health conditions by age. DALYs are a standard measure of disease burden. Figure from Whiteford et al (2013)
Consistent with our predictions, evidence from longitudinal studies in the United States and Europe indicates that major depression, PTSD and anxiety mostly follow adverse life events, implying that they are often a reaction or defence against those events. Typically, these adverse events involve loss, such as the death of a loved one, or loss of income and other resources. Other common adverse events involve intense social conflict, such as physical and sexual assault, marital conflicts and divorce.
Biological anthropologists and other mental health researchers have extended these findings to non-Western cultures. A study in Nepal, for example, found that exposure to violent conflict was associated with greater subsequent anxiety in a dose-response relationship; meanwhile, low socioeconomic status and nonconflict-related stressful life events were associated with an increased risk of later depression. Similarly, a longitudinal study in Ethiopia identified food insecurity as a risk factor for later elevated depression and anxiety symptoms. Around the world – from the Pacific Islands to the Arctic – colonised populations experience heightened risks of depression, suicide and substance abuse, which numerous studies link to poverty, culture loss and disruptive changes in traditional social roles. Our own research, based on data from hundreds of diverse cultures around the world, similarly indicates that suicidal thoughts and behaviours follow social conflicts, such as forced marriages, abuse and status loss.
In diverse cultures, people seeking the services of shamans and other local healers often complain of somatic problems, such as physical pain and weakness, but it’s revealing that in many cases they are dealing with social stress and showing classic signs of what Western psychiatry would view as anxiety and depression. In North African and Middle Eastern trance and possession cults, such as Zär in Sudan and Stambali in Tunisia, women and low-status men experiencing social stress – including conflicts with spouses or parents – exhibit somatic and depressive symptoms that are interpreted as possessions. The pattern across all this varied global research is the same: difficult emotional experiences that are pathologised by Western psychiatry tend to occur in response to environmental stressors that threaten the ability to survive and reproduce.
From an evolutionary perspective, it is logical that people today display strong negative emotional responses to forms of adversity that were common during our evolutionary history, such as status loss, death of social partners and physical attack. To survive and reproduce and pass on their genes, organisms must respond adaptively to dangerous environments, often by escaping them and learning to avoid them. In many animals, it is emotions that guide behaviours. Fear, anxiety, sadness and low mood are forms of psychological pain that probably serve functions that are analogous to physical pain – informing the organism that it is experiencing harm, helping it escape or mitigate harm, and stimulating it to learn to avoid similar harms. Psychological pain, like physical pain, probably evolved by natural selection, and in many or most cases is therefore not a disease.
Arguments against the ‘disease model’ of depression and anxiety, like ours, are often met with hostility or consternation. Disease model advocates argue that their approach reduces stigma by showing that the person is not to blame and by conveying the seriousness of their condition; they see alternative models as placing blame on the sufferer. But in fact the evidence shows that biological explanations of mental illness have not reduced stigma. Instead, what the disease perspective has done is distract us from talking about the source of most mental anguish: adversity, often caused by conflicts with powerful or valuable others, such as employers, mates and kin.
There are prominent voices within psychiatry who have shared our concerns. For instance, the American psychiatrist Robert Spitzer, chair of the DSM-III task force (the body charged with compiling the version of the Diagnostic and Statistical Manual of Mental Disorders published in the 1980s), wrote about his worries that the diagnostic criteria for mood disorders had resulted in substantial numbers of ‘false positives’: that is, healthy individuals who are responding normally to conflict and loss, who are then inappropriately diagnosed with a mental disorder. Allen Frances, chair of the later DSM-IV task force, has similarly warned that the DSM increasingly medicalises normal emotional reactions to life events.
Globally, depression is the largest contributor to the burden of mental ‘illness’ by far. If our hypothesis that depression is an adaptive, evolved defence is true, it wouldn’t offer much hope for a ‘quick fix’ or medical cure. Our ancestral lineage has grappled with adversity since before the dawn of Homo sapiens. It’s true that modern scientific knowledge has dramatically reduced some forms of adversity, such as child deaths. Also improving social norms, as advocated by the MeToo and the Black Lives Matter movements, can reduce adversity caused by abuses of power. But the reality is that some adversity is an unavoidable part of human life, caused by intractable conflicts of interest. If one person abandons her romantic partner for another one, for example, this is to her benefit and her ex-partner’s detriment. There is no way, at least in the short term, to make that better for the abandoned partner; nor is there a practical or fair way to prevent such strife from ever occurring.
In traditional societies, healers help to resolve psychological distress by resolving social conflicts rather than treating ‘mental disorders’. We believe that the wisdom of their approach is supported by evolutionary theory and a wealth of anthropological data. Just because psychological pain is unpleasant to the self and others, that doesn’t make it a disease, and we shouldn’t seek in the first instance to blunt it with drugs or other medical interventions. Instead, we should look to the social roots of adversity – to inequities, injustices and individual selfishness – and consider if and how we can harness mental anguish to help change ourselves, and other people’s lives, for the better.








