For many years, you struggle with impulsive and self-harming behaviours, and with intense emotional reactions – including when you perceive any signs that someone might be rejecting or abandoning you. You see psychologists, psychiatrists and other clinicians, but find no relief. Each clinician gives you a different diagnosis, and each diagnosis leads to a different treatment. You try what feels like a relentless string of medications.
Then, finally, a therapist diagnoses you with borderline personality disorder (BPD), and suddenly the pieces fit together. The diagnosis makes sense, and the treatment approaches designed for BPD start to help. You wonder why you weren’t told before that you had it. And while the diagnosis connects you with useful treatment and helps you understand your problems, you soon find that some healthcare providers seem to have negative reactions when you tell them about it. For example, they may seem less trusting of you, more distant or less willing to help.
Unfortunately, the scenario we’ve placed you in is anything but hypothetical for many people with BPD, and some readers will surely relate to it. As it turns out, BPD – which affects approximately 1 to 2 per cent of the general population – is one of the most highly stigmatised mental illnesses, even among mental health clinicians. Although stigma significantly impacts people with other psychiatric diagnoses, such as depression, schizophrenia and eating disorders, the stigma around BPD is particularly pernicious and worrisome. No disorder is met with more pejorative attitudes held both by clinicians and the public.
When people see mental health clinicians, they expect them to be nonstigmatising sources of knowledge and help. Yet the experiences of many people with BPD may not line up with those expectations. In past research, clinicians have reported feeling less optimism, less empathy and more hostility in relation to patients with BPD, compared with patients with other disorders. These negative attitudes and ideas may result in less effective care and lead some clinicians to avoid working with patients who have BPD. These patients already struggle with significant shame, negative self-concept and rejection sensitivity – stigma from clinicians is likely to exacerbate these problems.
Often, BPD is undiagnosed or misdiagnosed for many years due to this clinician stigma and misunderstanding. Some clinicians do not believe that BPD is a real disorder; others may be reluctant to give the diagnosis due to concerns that it could expose patients to stigma from others. The disorder can be diagnosed in both young people and in adults, and it is associated with significant distress as well as a substantial risk of premature death – by one estimate, around 10 per cent of people with BPD die by suicide. Early intervention is ideal. However, one study with structured assessments found that about a quarter of people diagnosed with bipolar disorder should actually have been diagnosed with BPD. In another study, the average gap between the onset of BPD symptoms and the time of diagnosis was 15 years. This suggests that if a person’s symptoms start to appear at age 15, they may not receive an appropriate diagnosis until they are 30. In that span of time, they will have spent most of their teenage years and young adulthood without a diagnosis that would have helped them conceptualise their problems and find treatment.
Making matters worse, media representations of BPD are often laden with stigma. Take, for instance, Glen Close’s character in the movie Fatal Attraction (1987), or the way that the BPD diagnosis was weaponised in relation to the recent court case between the actors Amber Heard and Johnny Depp – Heard’s speculated diagnosis was used to suggest that she must be a liar and an abuser. Moreover, materials seemingly meant to help people who do have a BPD diagnosis, including self-help books, often do more harm than good. Clinicians with experience helping people with BPD will commonly warn them that an internet search may uncover a litany of misleading ideas, including the notion that BPD is untreatable, which is directly disputed by decades of research on BPD treatments such as dialectical behaviour therapy.
Stigma is also entrenched in the legal system. Take, for example, California’s pretrial diversion programme, which provides treatment as an alternative to prison for people who have mental illness, with some exceptions. An effort is underway to change the programme’s exclusion rules – which currently bar people with BPD.
Why is BPD so stigmatised? The answer to this question is complex and not fully understood. However, BPD’s symptoms and the history of the diagnosis provide clues.
BPD includes a pervasive pattern of instability, also called ‘stable instability’. This instability affects mood and includes intense periods of anger or sadness that last anywhere from a few minutes to a few hours. Behaviour is also unstable, characterised by impulsivity and self-destructive acts. Similarly, people with BPD have difficulty with relationship stability and with finding a stable sense of self. They often oscillate between idealising other people and devaluing them – in one moment they might view a loved one as perfect and supportive, and in the next they might view that same person as awful or malevolent. This switch between idealising and devaluing others is called ‘splitting’, and often occurs when the person with BPD, who is usually highly sensitive to abandonment, perceives criticism or rejection.
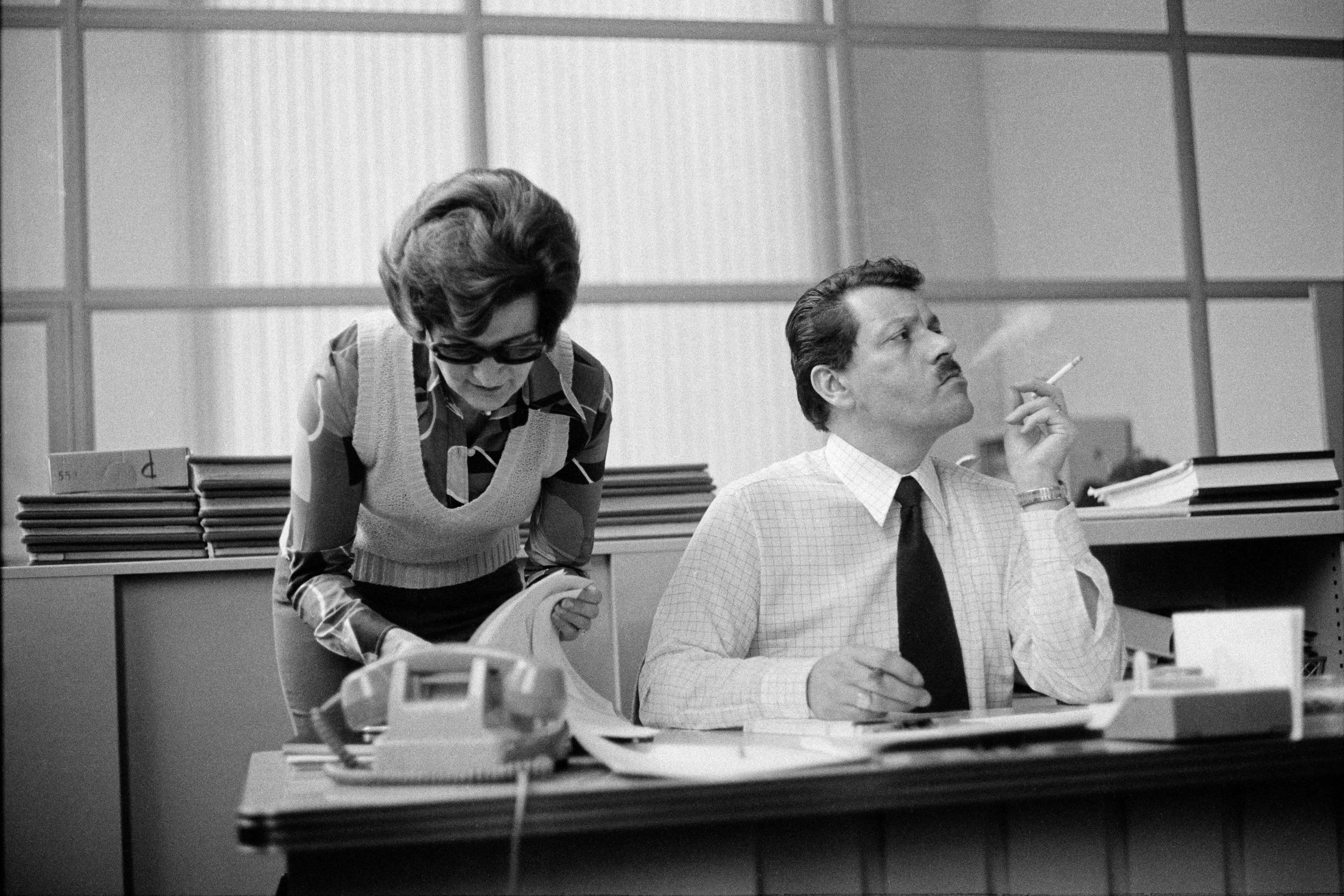
The term ‘borderline’ is difficult to understand and does not provide useful information about how we think about BPD today. It was first coined in the 1930s, and then was used pejoratively to label patients – mostly women – whom clinicians believed were untreatable, difficult or problematic. It has not been updated to reflect modern understandings of BPD. BPD was first officially recognised as a disorder in 1980, which catalysed research and treatment development. However, BPD research is significantly underfunded compared with research on other disorders, despite the fact that the disorder is common, impairing and life-threatening. The relative lack of focus on BPD is also common in training programmes, where many mental health clinicians do not learn about this condition specifically.
The symptoms of BPD may be difficult to understand for the public and for untrained clinicians. The ways in which these symptoms manifest are variable and unstable; this may make them seem within a person’s control, even when they are ultimately not controllable without treatment. While behaviours common in BPD – such as self-injury, suicidality and desperate avoidance of abandonment – are often seen by others as purposeful manipulation or attention-seeking, they are better understood as the result of overwhelming distress and emotional dysregulation. People with BPD are painfully struggling with these emotions and behaviours, and yet are often quickly assumed to have malicious intent because their behaviours can be difficult to understand.
Fortunately, however, the future is promising for people with BPD. Researchers and clinicians are working to better understand the disorder and the stigma related to it. In the coming years, the way that BPD and other personality disorders are conceptualised could change significantly. Some have argued that it should no longer be called a ‘personality disorder’. Moving away from the idea that someone’s personality is disordered may help others see this condition as something that a person struggles with, rather than who they are. In the public eye, prominent celebrities such as the US comedian Pete Davidson and the American football player Brandon Marshall have openly discussed living with BPD. The science of stigma suggests that such personal stories may be particularly useful for improving attitudes.
Against this background, there are things that you, too, can do about stigma, whether you know someone who has a diagnosis of BPD or you’d just like to support a change in how it is perceived.
Education can be transformative. Learning about one’s condition, often called psychoeducation, is itself associated with improved wellbeing and reductions in BPD symptoms. Psychoeducation is essential for reducing the stigma that many people with BPD internalise. If you or someone you love has BPD, seek education. A number of organisations offer free resources for learning about the condition. For example, Emotions Matter provides informational guides and online peer support. Similarly, the National Education Alliance for BPD has a wealth of online resources.
Organisations such as these also provide ample opportunities for patient and family involvement in educational seminars, conferences and advocacy initiatives. These can be empowering experiences. For those with BPD, fighting public stigma also provides an opportunity to combat their own internalised stigma.
Education about BPD is helpful for clinicians as well as patients: learning about the condition leads clinicians to express less dislike for people with BPD, more hope about recovery, greater willingness to treat people with BPD, greater empathy and compassion for them, and more confidence that they will be able to make an appropriate diagnosis and provide help. This suggests that stigma about BPD arises partly from misunderstanding and feeling unsure of how to approach treating the disorder. Although it is not a patient’s or a family’s responsibility to educate care providers, they can ask questions about a clinician’s training and attitudes about BPD when seeking care – and can seek a second opinion about diagnoses and treatment if necessary.
Finally, we can all aim to reserve judgment and seek understanding. People with BPD may often act in ways that seem extreme and difficult to understand to those without BPD. We encourage readers to consider that seemingly extreme behaviour is not always malicious or intended to harm others. People with BPD deserve to be understood, which might require reserving judgment and recognising that these behaviours often arise from painful struggles with emotion regulation. Connectedness and belonging are major themes within BPD recovery, and both are supported by an understanding, nonjudgmental environment.
People with BPD are vibrant, important members of our communities who deserve effective treatment and compassion. The stigma they often encounter creates barriers to care, and further entrenches feelings of shame. Deconstructing this stigma must start now – and it can start with you and those around you.