What does the term ‘personality disorder’ say to you? Based on the word ‘personality’, you might naturally infer that such a disorder must be connected to someone’s core self and persist over time, much more so than with other mental health problems.
If so, you wouldn’t be far off the official take in the latest version of psychiatry’s key text, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5, 2013), which defines a personality disorder as ‘an enduring pattern of inner experience and behaviour’ – a pattern that’s at odds with what is expected in a person’s culture, is ‘pervasive and inflexible’, and ‘leads to distress or impairment’.
There are 10 specific categories of personality disorder listed in the DSM-5. They include, for example, borderline personality disorder, with symptoms such as unstable mood, impulsivity and volatile relationship patterns, and narcissistic personality disorder, characterised by an outsized sense of self-importance and a need for admiration. What all the categories have in common, according to the formal criteria, is duration and pervasiveness in a person’s life.
As a psychiatric concept, personality disorders have been around since at least the 19th century, and they were included in the first edition of the DSM, published in 1952. However, in a recent paper, a research group led by the clinical psychologist Aidan Wright argues not only that the label ‘personality disorder’ is unhelpful and stigmatising – imagine learning you have a disorder that has to do with an essential, enduring part of you – but also that the concept is potentially misleading, both for anyone who receives a personality disorder diagnosis, and for the people who know them. The team think it’s time that mental health professionals adopted a new name and approach.
For starters, Wright and his colleagues argue that duration and pervasiveness don’t necessarily set personality disorders apart from other kinds of disorders. Wright points out to me that, in many cases of psychotic disorders such as schizophrenia, ‘those are also of a long-standing duration, and they impair people across domains.’ Similarly, ‘many cases of depression are also enduring,’ he adds. ‘Almost any disorder can show really long periods of duration.’ What’s more, research indicates that, in many cases, personality disorder symptoms improve over time rather than remaining stable indefinitely.
Perhaps more surprising is that, despite their name, personality disorders do not appear to be uniquely related to differences in personality test scores. Research highlighted by Wright’s team suggests that people showing more symptoms of a personality disorder tend to score higher on neuroticism and lower on conscientiousness, but no more so than people exhibiting symptoms of other psychiatric disorders – which undermines the idea that their condition is distinctively a disorder of personality.
If the kinds of problems that are today labelled as personality disorders are not generally more enduring or more tied to personality differences than other mental health conditions are, what does make them distinct? The answer, according to Wright and his collaborators Whitney Ringwald, Christopher Hopwood and Aaron Pincus, is interpersonal dysfunction – essentially, problems relating to oneself and other people – leading them to argue that the personality disorders should be recast as the ‘interpersonal disorders’.
If you look over the descriptions of the 10 main personality disorders in the DSM-5, you’ll find that they all include interpersonal problems. Among the markers of borderline personality disorder, for instance, is ‘a pattern of unstable and intense interpersonal relationships’. Schizoid personality disorder involves ‘detachment from social relationships and a restricted range of expression of emotions in interpersonal settings’; someone with the condition may have no desire for close relationships, and stick to solitary activities. Symptoms of narcissistic personality disorder include a sense of entitlement and a lack of empathy. And so on, for antisocial personality disorder (marked by disregard for others’ rights), dependent personality disorder, histrionic personality disorder, and the others.
That’s not the whole story though. Wright and colleagues emphasise that an interpersonal disorder is not only a problem with how someone behaves socially. It also involves ‘how the individual understands themselves and their motives, and pursues them,’ Wright explains to me. As he points out, these things are inextricable: how you think and feel about yourself and your goals shapes how you interact with others, and vice versa. For example, a person with borderline personality disorder will often feel ‘acute sensitivity to other people withdrawing from them,’ Wright says, ‘and they respond, oftentimes, with extreme efforts to avoid the abandonment that they perceive.’ That fear of abandonment may stem partly from the person’s negative or unstable sense of self. The overreaction to that fear, which might include panic or expressions of intense anger, can in turn have clear consequences for social relationships.
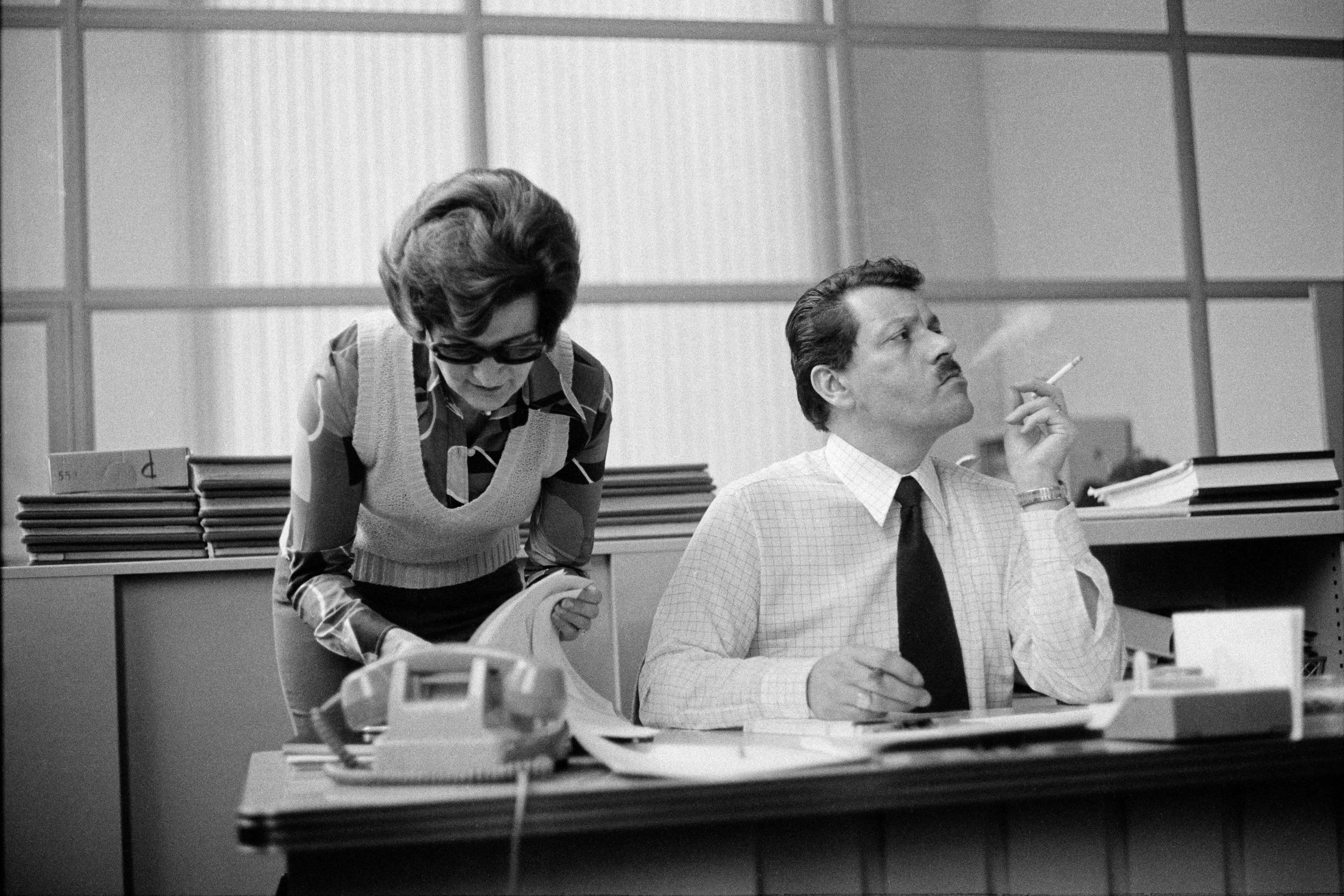
Of course, any mental health condition can have an impact on how someone gets along with others. A person with depression may experience an irritability or pessimism that affects conversations with family and friends. For those with anxiety or obsessive-compulsive disorder, worries and reassurance-seeking can infiltrate close relationships or the workplace. Indeed, when someone’s social anxiety is pervasive enough, Wright acknowledges, it’s ‘very difficult to distinguish from avoidant personality disorder’.
On the whole, however, he proposes that, for someone diagnosed with a personality disorder, interpersonal dysfunction is a more primary cause of the person’s problems than it is in other disorders. In depression, for instance, the social impact is ‘much more tail than dog’, he says – it might be driven by lowered mood and energy – whereas in someone diagnosed with a personality disorder, ‘it’s clear that the interpersonal is the dog.’
The labels used to diagnose disorders are more than a subject of academic or clinical debate; they matter to those on the receiving end. Replacing the term ‘personality disorder’ won’t erase a person’s fear of abandonment, passive or controlling behaviour, or other challenging symptoms. But reframing these conditions could, perhaps, improve how the affected individuals see themselves, and how other people – including mental health professionals – approach them.
While mental health professionals who’ve spent their career helping people with these conditions probably don’t view the term ‘personality disorder’ as pejorative, Wright says, some clinicians ‘use it as sort of a write-off term – as a way of saying, basically, it’s not worth your time to try to get far with [the patient], because their personality is just going to screw it up.’ In these instances, he argues, the term is used ‘to sort of blame the person for their problems’. For their part, individuals who receive a personality disorder diagnosis are often happy to have a name for their experience, he says. But there are some who’ve encountered the more dismissive use of the term, who ‘get that it’s pejorative and they don’t like it.’
Aside from reducing stigma about these conditions, the team write that it could help focus clinicians’ attention on ‘what is most important about this class of disorders for treatment, namely, that alliance difficulties’ – challenges a patient and therapist can have in forming a working partnership – ‘should be expected, and thus treatment should be modified accordingly.’
Efforts to reconceptualise mental disorders more generally (eg, as spectrums of psychological difficulty, rather than discrete disorder categories) have gained some traction among clinical researchers in recent years. Wright and his co-authors suggest their perspective is complementary to such approaches. And they are not alone in characterising the term ‘personality disorder’ as derogatory. In a brief paper published in 2022 on ‘improving the naming of psychiatric disorders’, the psychiatrist Bruce M Cohen and colleagues similarly floated the idea of replacing ‘personality disorder’ with ‘relational disorder’ or ‘relational difficulty’.
What Wright envisions as an eventual replacement for the current list of personality disorders isn’t a new family of labels such as ‘borderline interpersonal disorder’, but a more individualised descriptive process. It could be something akin, he says, to what the clinical psychologist Allan Harkness and colleagues have called a ‘review of systems for psychology and psychiatry’. Similar to how a physician checks on a person’s respiratory system, circulatory system and other systems of the body, a mental health practitioner might examine various areas of psychological functioning – including how a person is faring in the interpersonal domain.
Rather than learning that they have a particular ‘personality disorder’, a patient might learn that they have a form of ‘interpersonal disorder’ that is key to understanding their problems. If you were the patient, which message would you rather receive? By challenging entrenched ways of conceiving mental health problems, Wright’s group and others like them could be leading the way toward a more hopeful approach to treatment.