What my new patients mostly want to know from me is, can I help them? And, if so, how can my expertise as a therapist help? But what even is expertise in psychotherapy? My first inclination might be to tell a new patient: ‘I’ve done this for 20 years.’ But is expertise merely about experience? What happens in those years that leads to expertise? And what about education, training or therapeutic principles?
As a relational and psychodynamic therapist, part of the challenge in answering these questions is that I see each patient as one-of-a-kind. Therapy is a highly personalised affair – patients are eager to know how my approach might relieve their specific challenges, in a way that speaks to them.
It can be difficult to define ‘psychodynamic’ to a person who is new to therapy or unfamiliar with the term. Therapy involves, in part, understanding distinctiveness – how a patient sees things like no one else. If it were a matter of providing a simple ‘fix’, like a prescription, most would have figured it out already. What I am offering is far more personalised, as we define their problem together.
My therapeutic principles include collaboration, sustained investigation of patients’ experiences, confirming ideas with patients before drawing conclusions, and so on. But though my work is grounded in these principles, my expertise most often informs me of what not to do, such as making hasty conclusions rather than exploring the patient’s take on things. This is why I call myself a relational therapist, given my investment in experiencing the patient’s struggle in real time, opening the clearest panorama of the problem as they live it within their world (as I simultaneously work with my own feelings or ‘repetitive transference’ – a re-experiencing of earlier trauma, provoked by new interactions that resemble painful personal histories).
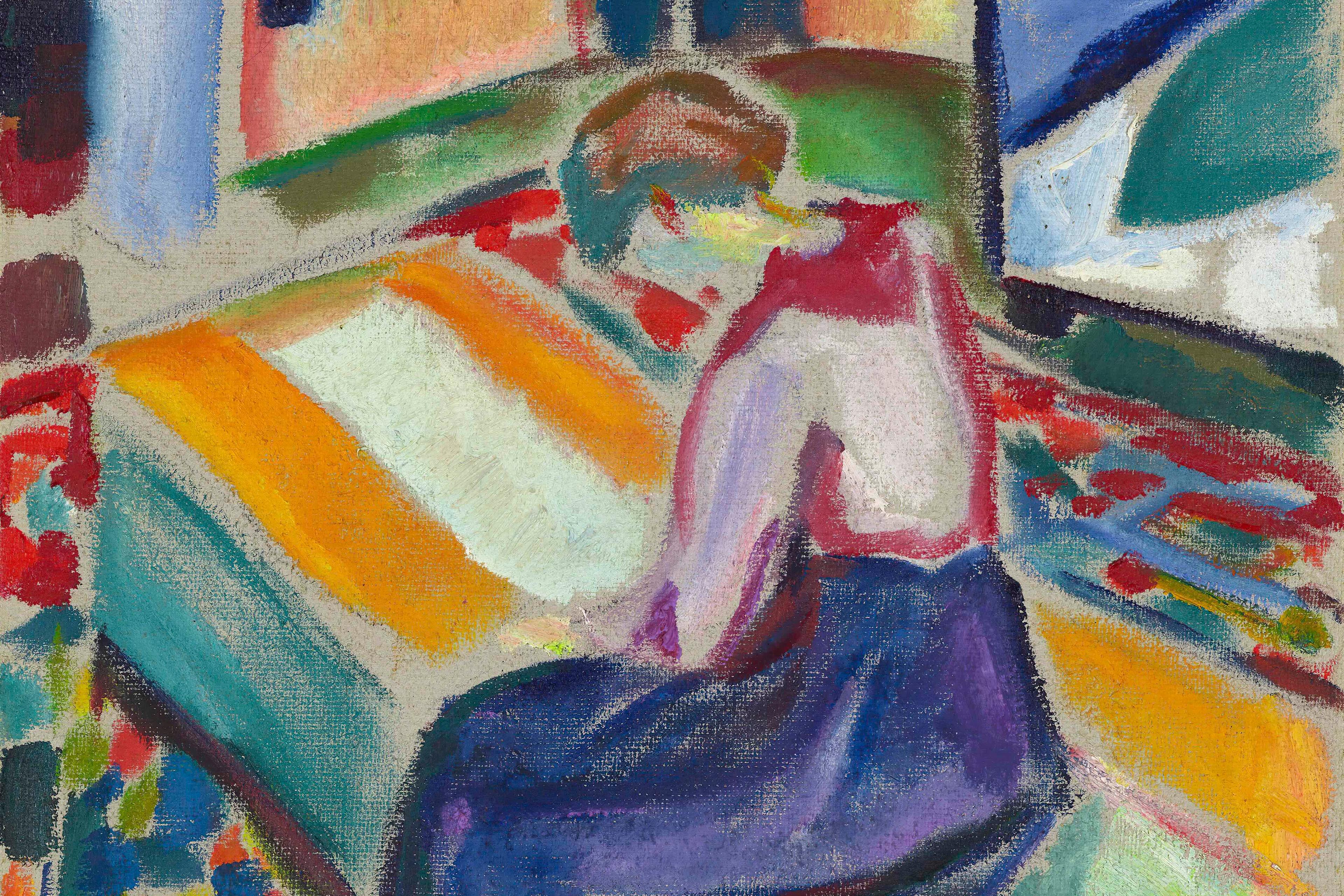
Psychology is an odd profession, a hybrid of the professional and deeply personal. Also, human relationships are complex and hard to distil. At first, I can state what works generally, but not specifically. How I connect with patients – my tone and style – is as crucial as the words themselves, just as music and lyrics combine in a melange of elements specific to each song. At a certain point, theory takes a back seat, as the relationship assumes a music of its own, our collaboration finding a distinctive syncopation.
The uniqueness of each patient is therefore expected but not predictable, even as popular notions of expertise suggest I should know what works in treating the mind. Expertise becomes a paradox, in my being certain of what I do not know but want to know. What does the patient seek, desire, fear? What has not worked in previous treatments? What do they think goes on in therapy, including between us? Meanwhile, I hope for patients to get a sense of my commitment to helping them find a greater freedom of thought, self-expression and relating to others.
All of this can mean different things to different people. At first, most patients are seeking relief amid traumatic anxiety; some long for sure-fire answers, for certainty. Notions of collaborating may not make sense. ‘C’mon, you’re the expert,’ they might say, ‘tell me what to do!’ Here I can explain my principles, but if patients have had reason not to trust those in authority, or never lived within a flexible relational world, my principles might sound abstract, like a new language or lyrics in a foreign tongue; it is often therapeutic action and attitude that speak the loudest. I have to earn a patient’s trust via my commitment and adaptability, and by communicating in ways that resonate.
I’ve experienced this from the other side. When I was new to psychoanalysis, struggling financially to finish my doctorate, my analyst agreed to reduce the fee until I completed. This went a long way toward convincing me that my analyst was as good-intentioned as stated. For other patients, such actions could include flexibility of scheduling, not charging for missed sessions in emergencies, or consistent patience, curiosity, even kindness. It is also affirming when I see a side of the patient that they may be ashamed of and welcome, rather than judge, that aspect of them. To paraphrase one of my mentors, Robert Stolorow, it all depends – upon the therapist-patient pairing, and on each patient’s unique understanding of therapy. The essential question is: ‘What does this person make of what’s happening?’ Some have never verbalised aspects of their emotional life with anyone.
I’m not saying to newer patients that therapy is simply a case of ‘Let’s give this a whirl and see what happens.’ Rather, I attempt to give a summary of what I believe myself to be a doctor ‘of’, tantamount to describing my view of the human psyche as existing within an embedded matrix of relationships. Close family, partners and friends are our mirror; we co-define each other; there is no ‘me’ without ‘you’. Patients reflect what they heard me reflect, with intermingling and often surprising results. Each of us has our own ways of hearing.
Often, we begin by co-defining treatment. How are we going to go about working on the problem, and what is the problem? Because I call myself doctor, many see me as offering a prescription. They believe I can cure depression rather than help them live with or transform it, and better understand which aspect of themselves is feeling so unhappy and isolated. Depression is often characteristic of a suffering long unexpressed or invalidated (with genetic, sociocultural, and other factors), a smouldering worthlessness for one whose emotions were disregarded. Such patients often devalue themselves, self-medicating with drugs, alcohol or sex.
I think we have become overly reliant on science for answers when it comes to the psyche. Some of my patients are dismayed to learn that treatment consists of a gradual working through, and not around, painful experience. The pain involved in this work can be ameliorated by any manner of interventions or support – eye movement desensitisation and reprocessing (EMDR), dialectical behaviour therapy (DBT), medication, yoga. But that pain is also an aspect of who the person is, of their reality and what they have lived through in torturous isolation.
Imagine a patient who is trans or of colour, traumatised by an institutional or societal bias then denied by those in power. Would we diagnose the patient as having a disorder? Wouldn’t we say the institution or society is traumatising or disordering? But then imagine I discover such trauma also evokes pain from an earlier abandonment or injury from their own caregivers – in which case the specifics become complex. This is further complicated by the blinders of my own race, gender and experience. Expertise here depends upon my deeply hearing this particular person, along with their feelings about me and my own inevitable blind spots.
Mental health symptoms are often gadflies, insisting that something is not right and needs attention, a child tugging at the sleeve. In listening to our problems, our problems listen to us and gradually speak the truth; possibilities expand, as patients both change and stay the same – the fusion of a new genre, instead of the same old pizzicato. I need to hear my patient first, hear the music of their experience – of their language games – and then see how we might combine.
‘Language game’ was Ludwig Wittgenstein’s term for the contextual meaning of words based on when, where and how words or phrases are put into play, which he saw as analogous to a game – the varieties of all possible games being as endless as languages and dialects. He once asked a colleague: ‘Can one play chess without the queen?’ He meant – if we take away that essential piece, the game itself changes. To me, the ‘queen’ of the ‘game’ of therapy is deep understanding, mutually found, with a focus on the dynamics of the relationship itself.
So, what I really want to know when I meet a patient is: ‘What kind of expert does this person need?’ This often speaks to the kind of help they seek, in contrast to what has come before. Wittgenstein also said that ‘to describe a language game is to describe a form of life’. A patient’s way of talking about their lives includes the background music of their lives. So I listen to their language: is it jumpy, lively, dark? Is the music lively, though the lyrics are grim or foreboding? Why are some notes hard to make out? To detour painful discord, patients may toil to drown out any undertones of uncertainty or suffering.
Even when I give practical behavioural guidance, I am offering new ways to talk and think about new ways of living – an ordering of dis-ordered notes, imploded often enough by trauma. If I address the problem with empathic directness, I wait to see if or how I’m heard. Again, what does the patient make of it? Are they asking me to help solve their problem by logic alone, a monotonous fugue numbing the ears? Do they hope I can provide the missing notes to alter the monotony? Or is that monotony pleasingly numbing?
Ultimately, my patients and I are co-synthesising and creating a more personalised genre, something distinctively scherzo or adagio, jazzy, pop-like or avant-garde. Can we find a good-enough rhythm? Can the patient come to hear richness in their own self-expression, notes of grief or longing? Or does our exchange leave one of us seeming tone deaf?
A scientifically minded reader might wonder how I judge whether the treatment is working. Progress needs to be defined and carefully understood. Usually, there’s more to it than ‘feeling better’. What often comes first is feeling different. One sign of movement is a patient’s reporting a more even blending of notes, rather than their soundtracks swinging uncontrollably from Taylor Swift to Igor Stravinsky. I am often curious what kind of notes patients want to play.
Often, the opening movement of treatment is but a beginning; once a patient feels heard and the initial fire is doused, there may be a long aria that comes belting through, after a lifetime of their being told to ‘zip it’.
I did not begin practising therapy in this way, by relying on seasoned intuition or spontaneity. Bill Evans, Miles Davis and Esperanza Spalding know music inside out, allowing them to play in their own inimitable way; such expertise inspires me as much as any analytic theorist. As one of my mentors told me: ‘We learn theory in order to forget it.’
An expert in psychodynamic therapy is like a well-travelled musician whose long, lived experience is heard in the notes. In this way patients entrust us to help them write a score all their own, now played in duet, after a lifetime of endless solo.