At various times, anxiety has been regarded either as a natural state worth embracing or as a central dimension of mental suffering. Anxiety disorders, such as panic disorder, generalised anxiety disorder, social anxiety disorder and specific phobia, represent an especially common way to think about anxiety in the 21st century – as something that is often pathological and worthy of treatment. The emotions that make up anxiety disorders are more elemental and more widely experienced: fear (an emotional response to an imminent threat) and, of course, anxiety (an emotion related to the expectation of a threat). There is a long-standing tension between the familiarity of anxiety as an emotion and the idea that such a common and even valuable emotion can be the basis of a pathology.
Though anxiety disorders are now considered the most common type of psychiatric disorders in the United States – affecting up to 31 per cent of adults at some point in their lifetime – anxiety hasn’t always stood out as a well-recognised mental health problem. In the US and elsewhere, the concept of anxiety has evolved over time in ways that have better allowed it to be seen as a major clinical concern.
Historically, anxiety has often been mixed with other symptoms in a way that has masked its significance. For example, in American Nervousness (1881), the American neurologist George Miller Beard outlined the causes of what he regarded as an epidemic level of fear in US culture. His specific diagnosis was ‘neurasthenia’. A significant part of the diagnosis included anxiety, but it also featured a variety of other psychological and physical symptoms, catalogued over long lists, including insomnia, heart palpitations and back pain. In part through Beard’s promotional efforts and popular writings, neurasthenia achieved considerable cultural cachet. The idea resonated as rapid social change was underway; Beard lay much of the blame at the feet of Thomas Edison and his inventions. As a medical diagnosis, though, neurasthenia quickly fell out of favour. Medical professionals began to doubt the seriousness of nervousness per se; they were inclined to regard other symptoms associated with it, such as cardiovascular complaints, as worthier of treatment. Beard himself contributed to this decline in arguing that this nervousness would subside as American culture grew more sophisticated.
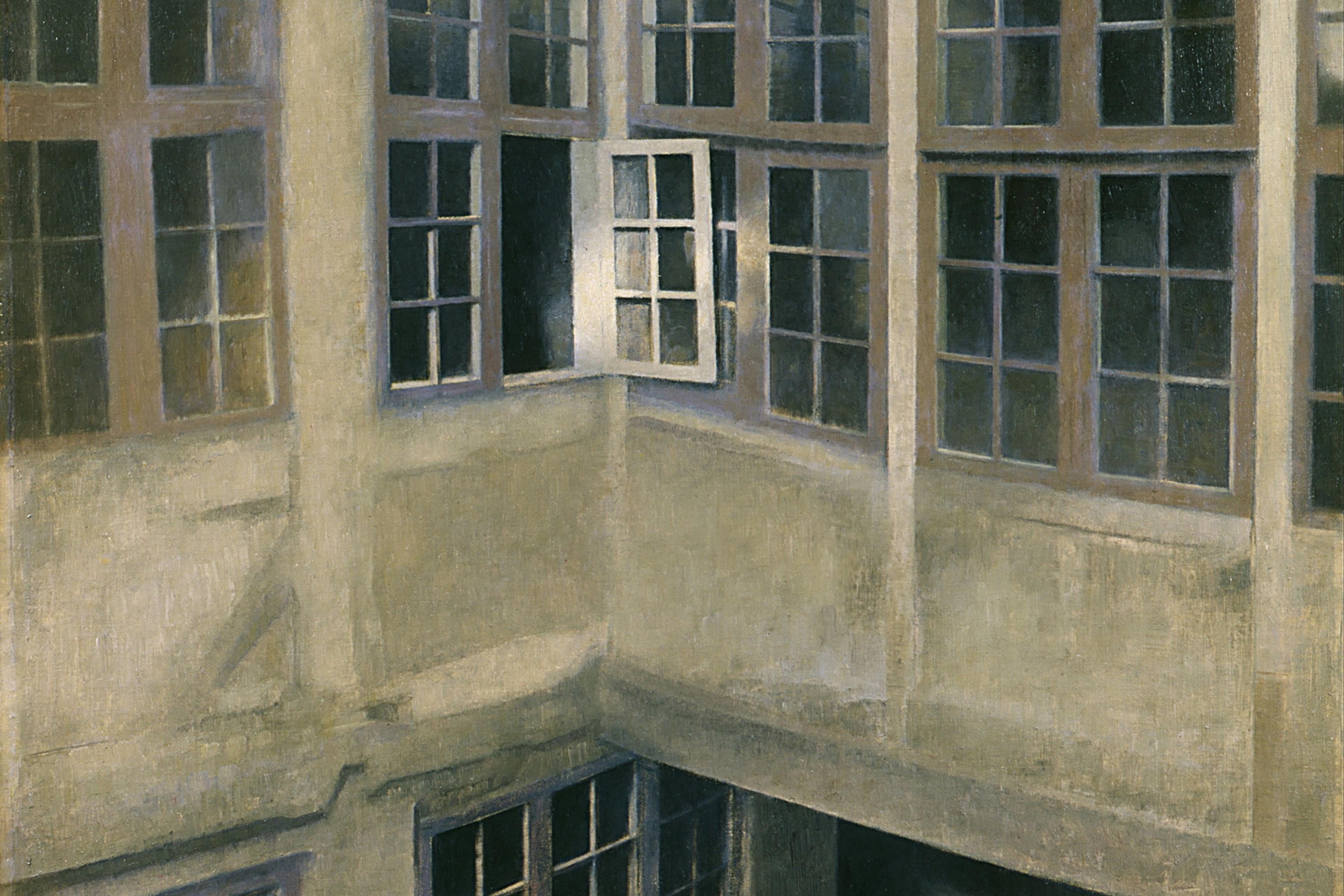
In the following decades, Sigmund Freud did much to renew the profile of anxiety, starting with an attempt to cleave it from the remnants of neurasthenia. He saw promise in the study of fear and anxiety, casting fear (and, by extension, anxiety) as the problem whose solution would throw a floodlight on mental life writ large. His followers took up this mantle, too, describing, among other things, some of the social circumstances that increase anxiety. In the middle of the 20th century, anxiety would again re-emerge as a significant concern and a cultural idiom of unease, the lens artists and authors used to talk about change. Perhaps the most famous statement in this regard was the book-length poem The Age of Anxiety (1947) by W H Auden – his locution persists to this day – though the poet was hardly alone in casting anxiety as the signature disorder of the era. In books such as The Meaning of Anxiety (1950) by Rollo May, psychologists and others saw much to worry about in the US, and the special value of talking about anxiety.
Anxiety also fit well within an emerging medical ecology. Miltown, an anxiolytic drug, was launched in the 1950s, ushering in a new era of seriously treating ‘nerve problems’, including the ‘nervous breakdown’ (of which anxiety was thought to be a key symptom). As a minor tranquilliser, Miltown was fast-acting and effective in calming nerves in a way that could seem miraculous. Advertisements focused on its ability to treat stress and anxiety, encouraging consumers to see their everyday unease in a new way – as a treatable condition.
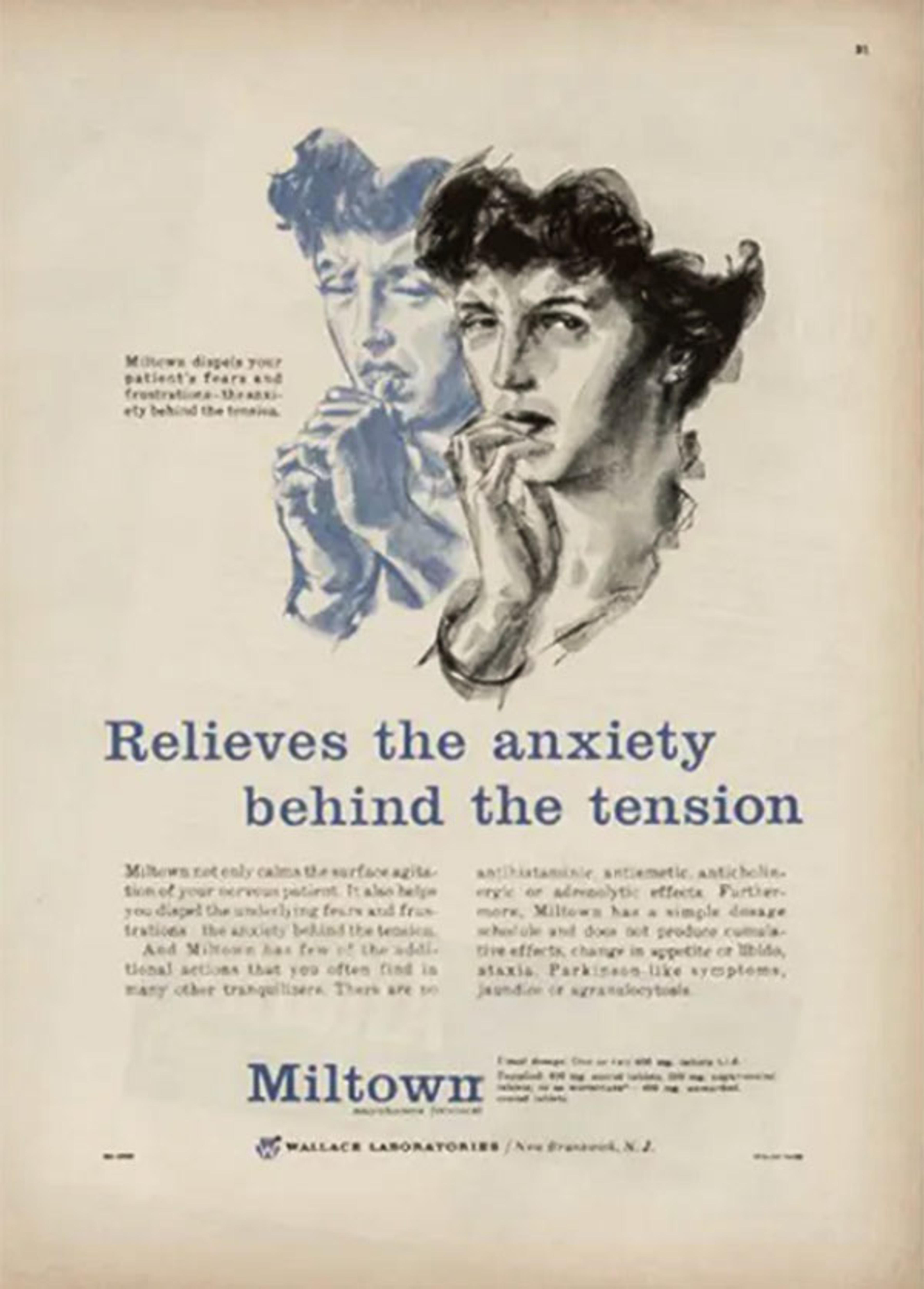
A Miltown advertisement from the 1950s. Photo via Reddit
But the mid-century age of anxiety would be short-lived. The rise and fall of Miltown was quick. Although much of the backlash focused on the drug itself, especially the potential for abuse, resistance ultimately circled back to the more elementary question of whether anxiety ought to be regarded as a problem to be treated with medication. Why treat something that was so common – and perhaps simply reflected the strains of an era in which anxiety really ought to be common? Evolutionary accounts, after all, begin with the idea that fear and anxiety enhance fitness by alerting people to potential threats.
Formal psychiatric nomenclature has, at times, approached anxiety with much of the same ambivalence. In the US, the Diagnostic and Statistical Manual of Mental Disorders (DSM) provides the symptoms and categories for formally diagnosing psychiatric disorders, and the place of anxiety in its pages has evolved over successive revisions. Anxiety was featured prominently in the DSM-II (1968) as a motif, apparent across a variety of disorders. The position of anxiety in the manual was not so different from what Freud had envisioned for it. But in DSM-III (1980) – an especially significant revision of the diagnostic criteria – anxiety was much less central.
DSM-III included a category of anxiety disorders, distinct from others. Yet the creation of the category did little to elevate anxiety’s prominence in research or clinical practice. The category included a wide and heterogeneous range of specific disorders, with no single anxiety disorder representing the category as well as, for instance, major depressive disorder would represent mood disorders. Generalised anxiety disorder seemed to work well in reflecting anxiety about many things, but the disorder is less prevalent than specific or social phobias. Research focusing on one anxiety disorder often had little to say about others. As a clinical target, anxiety was easily overshadowed by other types of disorders, falling to the noisy background of daily unease.
The creation of psychiatric disorder categories in manuals like the DSM is not merely an academic matter. The concepts that psychiatrists create tend to assume a life of their own once they are enshrined in diagnostic instruments and articulated as scientific tools. Due in part to the criteria provided in the DSM, the late 20th century could rightly be regarded as the age of depression. With the ascent of selective serotonin reuptake inhibitors (SSRIs) such as Prozac starting in the late 1980s, major depressive disorder assumed a special significance. By the DSM’s criteria, many people met the threshold for a major depressive disorder. And SSRIs seemed especially well suited to treating it. Around the time Prozac came on the market, the total number of doctors’ office-based visits per year for depression increased significantly, going from 10.99 million in 1985 to an average of 20.43 million in 1993 and 1994. It’s not that instances of depression suddenly multiplied. Instead – in an echo of the advent of early anti-anxiety drugs – depression was suddenly regarded and talked about by more people as a treatable medical condition, rather than as an everyday trouble that could be ignored.
Of course, anxiety never went away. Depression might have seemed ubiquitous, but people in the late 20th century hardly had less to be anxious about or more to be depressed about. Indeed, anxiety disorders frequently co-occur with major depression. Therapists have certainly recognised the importance of anxiety as a dimension of suffering in their patients: alleviating a patient’s fear and anxiety is the better part of making them well, even if targeting depression with SSRIs is the focus of much treatment. Furthermore, reported anxiety, as a basic emotional experience, began rising across birth cohorts during the 20th century – an increase that, I argue in my book Unnerved (2021), is due in part to changes in the family, a rise in income inequality and economic uncertainty, and increasingly fraught social attachments. If we’re in the midst of a new age of anxiety, the designation might very well be accurate this time.
As a therapeutic target, anxiety has risen in prominence again both because it is common and because it lends itself well to the 21st-century treatment armamentarium. Anxiety medications tend to be fast-acting, and the use of benzodiazepines, a powerful class of medications first prescribed decades ago, has increased over time in outpatient settings. Anxiety is also responsive to other kinds of treatment. It can be treated effectively with cognitive behavioural therapy (CBT), for example. And CBT can be administered in a variety of settings, without necessarily requiring extensive training. In school settings, for instance, anxiety interventions can be administered effectively by nurses and teachers. Patients presenting psychiatric symptoms to doctors have increasingly been presenting anxiety.
Some of the long-standing uncertainty about whether anxiety is worthy of treatment has been resolved as well. It is increasingly clear that even though a degree of anxiety might be natural and perhaps even essential to a well-adapted species, anxiety also has negative consequences with respect to role performance and wellbeing. Anxiety can undermine school performance in children and adolescents. Anxious workers are often less productive. Anxious athletes might not perform up to their own expectations. Over time, anxiety could lead to worse physical health, too.
Although there remains considerable stigma attached to most psychiatric disorders, for anxiety, it is different and shifting. It is possible to regard anxiety as both treatable and not at all unusual. Much of the enduring stigma surrounding psychiatric disorders centres on a fear of violence. But in the mind of the public, anxiety is less associated with violence than, for instance, schizophrenia is. The lingering stigma related to anxiety is partly due to the idea that it reflects weakness. An old theme that has fed into the ambivalence over treating anxiety as a clinical problem is that people can overcome it with the right mindset and might even learn from it. Yet there is growing acceptance that psychiatric disorders are largely genetic in origin, diminishing the stigma once attached to disorders that were previously regarded as a matter of weak character. It is likely easier now to admit to others that one is anxious.
The idea of an age of anxiety is rarely intended to be a specific psychiatric claim. But there has been an increase in the seriousness with which anxiety is taken as a clinical concern among both the public and treatment providers. If we’re more anxious now than we used to be, we’re also more inclined to treat our anxiety. In that sense, the age of anxiety has been slow in coming but it might be here.