The second time I meet with a new psychotherapy patient is when I take their history. To help them look ahead, I need an understanding of what’s come before. People don’t often talk about their life from birth to the present day, in that order, and giving them the opportunity to do so can be powerful. It can lead to an appreciation of how much adversity has been overcome; a revelation that current troubles were presaged by older, half-forgotten ones; an emergence of defences that have gone unchallenged for who knows how long. But sometimes asking for a history leads a patient to a different, more disturbing realisation: that they don’t have one.
Living without history is a serious condition, though it’s not listed in any diagnostic manuals. What you’ll find instead are misleading descriptions of the condition known as borderline personality disorder (BPD).
BPD is what happens when a person is denied a history. Despite the common notion that the disorder emerges chiefly due to genes or temperament, there is a necessary environmental component. As children, people who go on to develop BPD tend to exist in regular states of invalidation and confusion, often due to chronic abuse or neglect. The instinct to survive – to predict catastrophe at the hands of an unpredictable authority figure, say – takes up the space that might otherwise be devoted to learning who you are. Eventually, BPD binds a person to the present, so that every feeling seems permanent, every thought inescapable. The old wounds remain open even as time passes, and one lacks the words to describe them.
‘Weird.’ That’s the word that my patient, a 34-year-old event photographer whom I’ll call Rose, used when I asked her to describe her childhood – one of my standard enquiries when taking someone’s history.
‘How was it weird?’ I asked.
‘I don’t know,’ she said. ‘I don’t know.’
The word kept reappearing as we talked. It was weird when Rose’s parents divorced in her early childhood, and weird again when, a few years later, her mother suddenly became a devout Catholic. It was weird to be pulled out of school multiple times over the course of a decade as Rose’s mother forced her to attend increasingly strict parochial schools. Being alone in a room with her father still felt weird.
Rose didn’t have amnesia, the condition of being without memory. Being without history, as I have found over a decade of working with patients, is far more insidious. It meant Rose had been robbed not of memory itself but the connective tissue that gives memory meaning: the understanding of cause-and-effect, of why something happened in the way it did, how it made her feel, and how those circumstances and feelings informed what happened next. Her narrative felt like a jumble of scenes from a hastily edited film, roughly in order but stripped of emotional language to ground Rose in the story of her own life. She felt wary and frightened of her ‘weird’ feelings about her father, for instance: had he done something terrible to her that she couldn’t remember? Or was his coldness, his frequent absence, and the verbal abuse he levied toward her mother enough to explain the way she felt?
People with BPD are often blamed when their treatment isn’t working
Rose’s treatment history also felt weird to her. ‘It’s like I don’t belong anywhere,’ she said to me. Following a series of brief, largely unhelpful therapies in her 20s, she’d begun a course of cognitive behavioural therapy (CBT) two years earlier, after increasingly agitated moods and self-loathing thoughts made it nearly impossible for her to work. But after a couple of months, Rose’s therapist said that her attitude was too ‘combative’ for their therapy to be effective, mostly because Rose often pushed back on the therapeutic ‘homework’ her therapist assigned. So, she was referred to dialectical behaviour therapy (DBT) – a CBT variant often described as the gold standard for people diagnosed with BPD. Here, in a mix of individual and group sessions, Rose found that she wasn’t combative enough.
‘My therapists expected me to be difficult and self-destructive, but I tend toward people-pleasing,’ I recall her saying. ‘They taught skills focused on problems I didn’t have, for people who cut themselves or threaten suicide.’
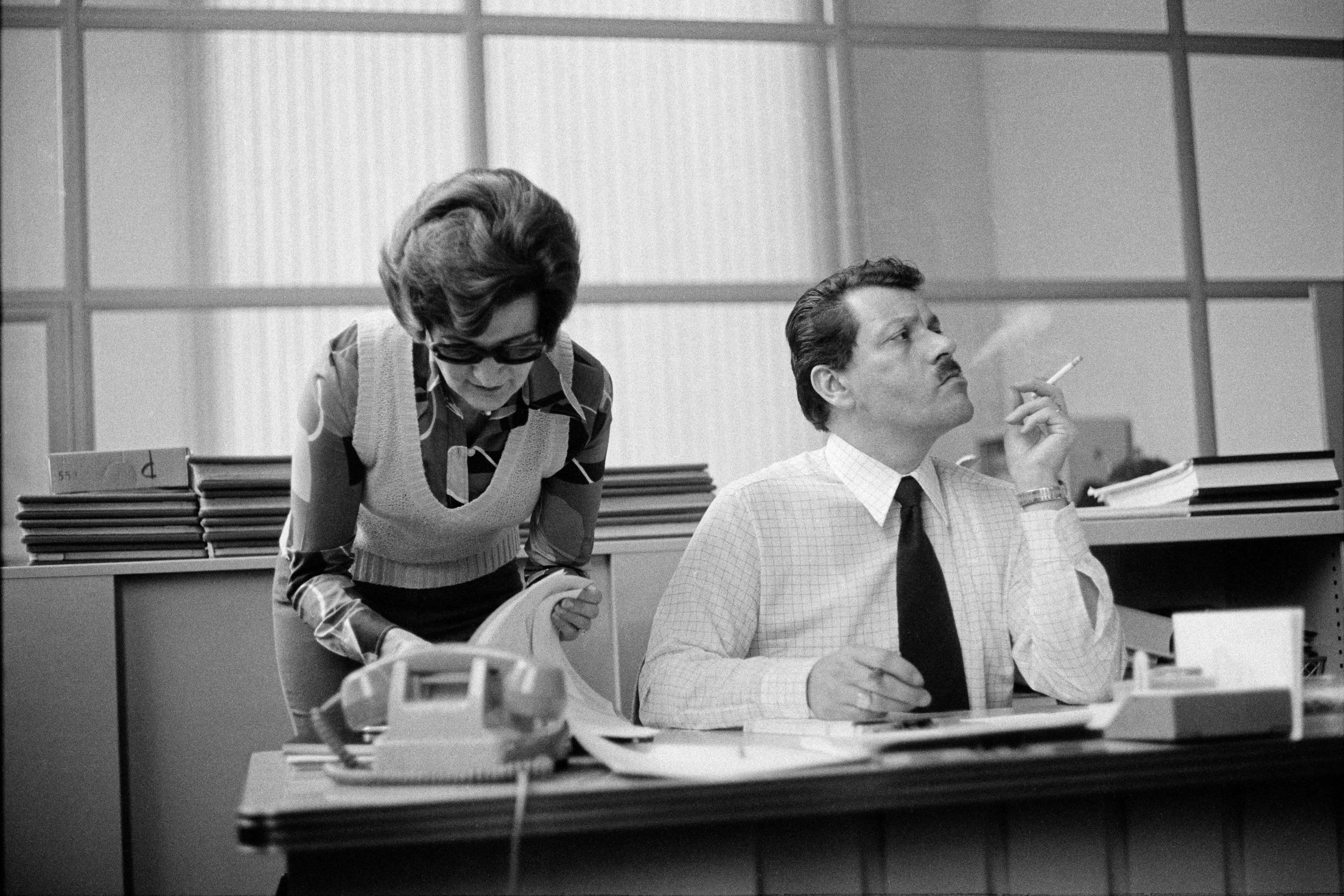
These types of behaviours are what most clinicians and laypeople associate with BPD. They are in line with the depiction of wild, provocative people – often women – that dominates the mainstream view of the condition, which focuses more on what can be observed from the outside than what it might feel like from the inside, or how someone’s experience came to be that way. In much popular and, regrettably, professional literature, BPD is also portrayed as a hopeless condition. The patients are seen as too difficult, too manipulative, their behaviours too scary. As Rose experienced, people with BPD are often blamed when their treatment isn’t working.
What Rose didn’t know at the time – what even most mental health professionals don’t know – is that the BPD diagnosis itself has also been severed from its own history. This severance has perpetuated a cycle of stigma, shaming, and experiences with treatment that can be inadequate or harmful.
The term ‘borderline personality’ was popularised in professional circles in the United States in the 1960s, largely through the work of the psychiatrist Otto Kernberg. Kernberg drew on nearly a century of psychoanalytic theory and research, which at the time was the dominant perspective in US psychiatry. He portrayed BPD as existing on a continuum that ran from the psychotic on one end to the neurotic on the other. Under this model, many people we would call ‘normal’ fell on the side of neurosis; they had internalised the rigid strictures of society and found ways to function within them.
In Kernberg’s description, people with the ‘borderline’ condition often led lives indistinguishable from their neurotic counterparts – engaged in the outside world of relationships, careers and so on – but they could also veer into emotional states untethered from that world, states in which they felt persecuted or empty, leaving them frantic to escape through any means available, such as substance use, self-harm or explosive interpersonal conflicts. A body of work from Kernberg and others grew through the 1970s, discussing novel ways to help these individuals, who had often been misdiagnosed and mistreated in the past.
This work was not perfect. Kernberg saw BPD as dispositional in nature and left little room to consider the role that early trauma and abuse played in its development. But a foundation existed to understand BPD as something treatable and connected to broader human experience.
Clinicians and the media seized on these salacious features until they came to all but define the disorder
Then, US psychiatry took a sharp turn: the psychiatric establishment chose to abandon psychoanalytic language and principles in favour of a model of illness based on concrete behavioural observation. The third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), published in 1980, reflected this sea change, which would radiate out to influence other diagnostic texts, such as the International Classification of Diseases (ICD).
Though its description of BPD kept the word ‘borderline’, the DSM-III made no mention of what that word actually meant. The manual instead depicted BPD as a bullet-list of symptoms, many of which were behaviours – like cutting, substance abuse or suicide attempts – that are indeed elevated among people with BPD, but that many patients (like Rose) don’t engage in. Both clinicians and the media seized on these observable and salacious features until they came to all but define the disorder. This, in turn, obscured a broader understanding of the internal experience of BPD – the intense emotion and the sense of being cut off from oneself – that is its most disturbing part, if you ask people who actually carry the diagnosis. It is also what connects BPD to the rest of the population. Almost anyone can, at times, relate to the experience of feeling overwhelmed, or the urge to look to others to define who we are, or the wish to suddenly become someone else. BPD is a facet of the human condition pushed to its extreme, but what’s too often depicted instead is an out-of-control, difficult person.
DBT emerged in the wake of the diagnostic changes, and this form of therapy treats behavioural control as its central goal: the effectiveness of its exercises, even those geared toward improving emotional regulation, is evaluated based on how much a patient decreases visibly destructive actions. For some, this feels like an apt approach and the treatment is helpful. But for others, including Rose, it can perpetuate the idea that they don’t belong anywhere.
New forms of psychological treatment emerged in the 1990s and 2000s centred around an increased understanding of the role that chronic trauma plays in development. Yet, even to this day, it is not widely recognised that BPD is a condition rooted in early aversive experience, including trauma. Our system of diagnosis is too rigid – too neurotic, we might say – to expand our understanding of BPD beyond the surface level.
Fortunately, recent years have seen efforts to weave BPD back into the broader history of mental illness and treatment. A modern adaptation of Kernberg’s work, known as transference-focused psychotherapy (TFP), has been developed and empirically validated. TFP uses the patient-therapist relationship itself as means to understand and change a patient’s tendency to recreate maladaptive patterns in how they relate to the self and others. Mentalisation-based therapy (MBT), another tested approach that combines ideas from psychoanalysis, developmental psychology and trauma theory, emphasises the cultivation of reflective inner space. Patients are taught how to consider multiple possibilities in times of distress – for instance, how to turn a thought such as ‘I know they hate me’ into ‘Perhaps they hate me, or perhaps there’s another explanation for why I feel this way.’ This approach reflects an appreciation that much of the borderline experience involves a sense of being trapped in a terrifying reality.
These therapies are not yet as widely available as DBT and others from the CBT framework. And it has been difficult to break through an entrenched stigma that BPD is something other – something difficult and combative. Perhaps even more, it has been difficult to convey that BPD is not the same for everyone, and so we need multiple types of treatment to suit the individual, rather than demanding the individual conform to one rigid treatment.
My approach to working with people with BPD pulls from multiple sources, including TFP, MBT and DBT. This attempt at pluralism was part of why Rose felt our work together was ultimately helpful. ‘I needed to feel like you knew how to help,’ she once told me, ‘but also that you were open to not knowing, to learning who I was outside of the BPD label. I didn’t know who I was either, and I needed the space to figure it out.’
There is hope in understanding BPD as the result of history denied. Not only the hope that patients who suffer can come to lead fuller, stabler lives, but that the rest of us – people striving toward a society of greater peace and compassion, no matter where one falls on the spectrum of mental health – can come to appreciate how important it is to connect past with present.